A while back I mentioned I’d aim to write a longer post on Long Covid and Katja Grace’s post on it. This is that post. First I deal with Katja’s post, then Scott Alexander’s Long Covid: Much More Than You Wanted to Know.
My core model of Long Covid after writing this post:
Long Covid is real, but less common than many worry it is.
Reports of Long Covid are often people who have symptoms, then blame them on Long Covid whether or not they even had Covid. The exception is loss of taste and smell.
Long Covid severity and risk is proportional to Covid severity and risk.
If you didn’t notice you had Covid, you’re at very very low risk for developing Long Covid.
Vaccination is thus highly but incompletely protective against Long Covid.
Children are thus at minimal risk.
Omicron is thus less likely to cause serious Long Covid than Delta.
My current estimate of the forward-looking-practical-use chance of a healthy non-elderly person getting serious, life-impacting Long Covid from a case of Omicron is about 0.2%, or 1 in 500. This number will decline further once Paxlovid is readily available.
Long Covid remains the primary downside of contracting Covid while young and healthy.
Diseases often have long-term negative health effects. Long Covid is not fundamentally so different from Long Other Disease. If you are worried going forward about Long Covid you should consider things like permanently not living in a city to avoid diseases.
A lot of people are in poor health. It is likely worthwhile to treat your health a lot more seriously than most people do, irrespective of Covid.
The Precautionary Principle carries some weight in all this.
Remember that the chance of preventing a Covid case via additional Covid prevention, going forward, even with extreme measures, is not all that high.
If you compare the potential costs of Long Covid to the costs of Long Covid Prevention, it is obvious the second is a bigger threat.
Short-term additional vigilance is reasonable but rapidly becoming less reasonable.
Using Long Covid as a reason for not returning to normal once case levels come down would not be reasonable.
Katja’s Post
This may or may not be entirely fair, but I am going to use Katja Grace’s post on LessWrong as a steelman of the case for worrying about Long Covid. It is by a thinker I respect, and is clearly advocating for the side of ‘be worried,’ and seems to aim to be exhaustive. It doesn’t cover every concern I’ve heard, but it’s a lot of them.
I’m placing sufficient stock by her selection process that I will focus in detail on the ones she includes.
Katja assigns letters A-R to her points, and I deal with these in order. Before I begin, I’ll summarize my takeaways so you can decide which sections you want to read or skip, and have perspective on what you are reading, if you want to go in non-blind.
A, B, C and D establish that Long Covid exists but don’t make the case about frequency or causation that they might seem to be making. They do establish that a lot of people have a lot of chronic health conditions.
E is effectively punted to the section on Scott’s post since it talks about Scott’s estimate.
F, G and H are a claim that there is a bunch of ‘dark matter’ style damage being done and that it manifests in lots of additional deaths that aren’t attributed to Covid. The population statistics don’t match up with this, and I consider these to be selection effects or otherwise non-causal.
I reminds us that lesser outcomes can also be concerning but I don’t see how they can be that big a share of the overall problem.
J asks about future unknowns. Given how much time has now passed, and what I see as the relevant reference classes, I don’t think we need worry about this going foward, but precautionary principle does apply.
K deals with the French study that says that Long Covid is correlated with thinking you had Covid but not with Covid itself once you control for whether you think you had it, but when you only check Covid versus symptoms you still find the correlation. I agree with Katja’s claim that mostly this isn’t psychosomatic, but I do continue to think a lot of it is ‘blame whatever is wrong with me on Covid.’
L, M, N and O say already established true things but those facts don’t seem to provide evidence for Long Covid being concerning.
P actively seems to go the other way.
Q doesn’t seem relevant to the calculations that matter.
R has logic I disagree with, and to extent it was a consideration I think it is no longer one.
The key question with all her points is what you’d expect to find in various different worlds that have different severities of Long Covid.
A. Really bad anecdotes aren’t hard to find.
This is strong evidence in the sense that if we couldn’t easily find really bad anecdotes, we could be confident that Long Covid wasn’t a Thing worth worrying about.
It’s also strong evidence that people believe that Long Covid is a thing.
Beyond that, it’s not strong evidence, because a large percentage of people have had Covid, more people than we realize get long-term debilitating health problems from a range of causes, and anyone who experiences long-term debilitating health problems during the pandemic is likely to consider blaming them on Covid.
Similar things happen for example with Lyme disease. The degree to which Long Lyme is a real thing is similarly disputed, but there’s little doubt that a lot of people will claim they’re suffering from Long Lyme who very clearly are not.
Another key question is where the anecdotes are drawn from. It is not surprising that Katja can receive a response to a bat signal put up on the internet – her social vicinity matters more, so I’m more interested in B than A.
B. Bad anecdotes are common enough to show up in my vicinity
Katja uses the plural in the title. She cites two anecdotes here, that of Michael Osborne from her extended network, and the claim of a distant relative. As she notes, the distant relative was sufficiently distant that she didn’t hear about them having Covid first, and only mentioned it due to the Long Covid discussion, which is a far larger network and involves a much lower reporting threshold.
It seems that Michael ended up recovering, so it wasn’t lifelong, but this sounds a lot like losing a year and a half of one’s life. It’s really bad, bad enough that his account went viral on Twitter.
For reference later, Michael got Long Covid in March 2020, so on average it was more likely severe, wasn’t treated as well as we can now, and he was certainly unvaccinated.
So the question becomes, how many people does Katja know as well or better than Michael, and also to what extent knowing Michael caused Katja to write the post and have her concerns.
As an additional data point, in my fully extended networks, I have two examples of Long Covid. One is also from someone who was of a broadly similar age, in excellent shape and did a ton of exercise. Not as bad as Michael, but a major hit to their long-term health that they strongly believe is due to Covid. The other is someone older, and I don’t know what happened there beyond a vague claim, it’s a very weak connection and we haven’t communicated in almost two years now.
Also noteworthy is that both of those cases were from March 2020.
If I was quickly ranking how striking hearing about a given person’s case of Long Covid would be to me, I’m guessing the younger of these cases was somewhere between 50th and 200th most potentially salient, and the older one between 200th and 1000th. I don’t know how many people fall into ‘I would have heard about it at all’ but I’m guessing the number is in the low thousands.
There’s also a third potential case, but the person in question already had other chronic conditions, and claims to have had Covid three times but never got a confirmed Covid diagnosis. I am skeptical.
Other than those cases, I don’t know of anyone claiming they have serious Long Covid that I know personally.
So overall, this seems like evidence that things that seem like Long Covid do happen, but it doesn’t seem especially strong or scary with respect to frequency.
C. Rates of ambiguously-maybe-quite-bad symptoms seem very high, even for people who only had mild Covid
This Norwegian study, n = 70k, has, for mild cases (in a sample mixing people who had Covid 1-6 months prior with people who had it 11-12 months prior):
10.2% with fatigue (6.4% higher than control in the 11-12 months case),
7.1% with poor memory (3.5% higher than previous control),
9.2% with brain fog (5.3% higher than previous control).
6.9% with shortness of breath (5.6% higher than previous control)
Huge if true.
That’s among the unvaccinated – she estimates based on other studies that vaccination cuts this in half.
As I said when I first saw this study, these results would show up at the population level. The United States has had 61 million official Covid cases, and at least two thirds or so of cases are missed. The majority of Americans have had Covid. A lot of those are from December 2021 and January 2022 so it’s too soon to know their long-term outcomes, but even excluding them we’re looking at half the population, so going from 4% to 7% fatigue, 1.5% to 4% shortness of breath and 4% to 7% brain fog, if it was all happening at once and symptoms are frequently long-term or permanent. I believe these are snapshot numbers. But given the correlation between different symptoms is imperfect, and how often the polls I’ll get to shortly showed that these symptoms interfere with the ability to work, this is a very large set of claims, enough to materially decrease the size of the productive workforce.
Does the anecdata above match several percent increases in a large number of distinct symptoms? No, it doesn’t. People are primed by their Covid to look for problems that aren’t there, or are barely even there, or were caused by something else.
As Katja notices, these numbers imply that a lot of people can’t work.
As an experiment, I did a poll while writing this asking if people (1) had Covid and (2) if they currently have at least one of the four symptoms above – fatigue, poor memory, brain fog or shortness of breath. Every study says there’s a correlation between such symptoms and self-reported Covid but I’m curious as to magnitude in practice. I expect this to be true regardless of whether there’s a substantial causal link, both because the studies say there is one, and because I expect people to be more likely to notice such problems if they have Covid and to think they have had Covid on the basis of now having such problems.
So the real question here is the size of the correlation.
Early results had things reversed a bit, but this makes more sense. Here are the big observations.
Wow, that’s a lot of people reporting those symptoms. Like, a lot. 29%!
By comparison, even if there was zero overlap, the Norwegian study said 22%.
Of those that report having had Covid, 29% report symptoms.
Of those that report not having had Covid, 27% report symptoms.
That’s ‘not significant’ in both senses.
This is not a scientific study but it also really is not compatible with rates doubling or more.
Also, in terms of how big a deal this is:
So what we do know is, these kinds of problems are a really freaking big deal in general. Almost 45% of those who report these symptoms say they’re wiping out half of their ability to work, and 29% of respondents reported the symptoms in the other poll, so this is at more than 10% of all productivity lost. And for a quarter of all people, at least one of these is being reported as a big deal.
Once again, not a scientific study or representative sample or anything, but ouch. Seems worth exploring this more. Also, I realized I don’t know how to thread polls in Twitter’s interface, someone in the comments clue me in please for next time.
D. It looks like a lot of people can no longer do their jobs
If a lot of people can indeed no longer do their jobs, and we can be confident this is due to Covid, then this is a big deal.
Katja starts with this, accompanied by bar charts.
Katie Bach of Brookings argued a few days ago that an estimate of 1.1 million people out of work because of long Covid is reasonable, out of 103 million working age Americans she estimated had had Covid, i.e. a roughly 1% chance of being entirely out of work
But that’s Katie’s estimate and not an actual argument or evidence.
Her second source is a Washington Post article I’d seen before claiming lots of people were out of work due to this problem.
Hard data is not available andestimates vary widely, but based on published studies and their own experience treating patients, several medical specialists said 750,000 to 1.3 million patients likely remain so sick for extended periods that they can’t return to the workforce full time.
Long covid is testing not just the medical system, but also government safety nets that are not well suited to identifying and supporting people with a newly emerging chronic disease that has no established diagnostic or treatment plan. Insurers are denying coverage for some tests, the public disability system is hesitant to approve many claims, and even people with long-term disability insurance say they are struggling to get benefits.
…
The Washington Post interviewed more than 30 people around the country experiencing the sudden financial slide caused by the long form of the disease.
…
“I have hundreds of patients who have had to take time off for long periods of time, quit their jobs, or get fired from their jobs, or take lesser-paying jobs” because of long covid, said Janna Friedly, vice chair for clinical affairs at the Department of Rehabilitation Medicine at the University of Washington School of Medicine, where she and her team are helping long haulers build strength and return to work.
…
John Buccellato, 64, an emergency medicine doctor at an urgent care clinic on Manhattan’s Upper East Side, was hospitalized with the virus in March 2020, in the same hospital where his mother died of covid.
…
Chimere Smith, 39, a middle school teacher in Baltimore who has testified in Congress about covid’s impact on her life, has not worked since she caught the virus in the early weeks of the pandemic.
…
The Social Security Administration said in an email that it has received 16,000 covid-related disability claims since December 2020, but the agency would not disclose how many of those were approved or denied.
…
She said she was laid off in March 2020. Shegot covid eight months later and has been plagued by fatigue, shortness of breath, joint pain and spikes in body temperature ever since.
…
Hood got sick with covid in October 2020, forcing her this year to close the small business she had run with a friend for 15 years, selling wigs, specialized clothing and other needs for cancer patients. Hood’s attempt to return to the job she loved ended in frustration.
…
Two months after the September [2020] birth of her baby, Leon, she tested positive for the coronavirus.
I list all the article’s anecdotes both to illustrate that the article is largely a long list of such anecdotes, and also to note the times of infection. Two were again very early (March 2020 and ‘the early weeks’) and the others were all in 2020 as well. To which you could say, sure, it takes time to call Long Covid long and for financial distress to overwhelm you. But there really weren’t that many cases in March 2020. What stands out about March 2020 is that cases were on average more severe and we had both poor understanding of how to treat Covid and a lack of hospital capacity. If lots of our examples of Long Covid also come from that early, we should be skeptical that the risks are similar going forward.
Janna Friedly specializes in treating such patients, and they often get referred to her, so her seeing many such patients may not be indicative of a general public health pattern. Similarly, the ‘many medical specialists’ estimate here is the kind of thing that tends to be inflated for various reasons, and also that doesn’t come with any method, reasoning or data attached.
The only data we get here is the 16,000 disability claims related to Covid since December 2020. Is that a lot? About 500,000 disability claims are filed each quarter, and it’s been four quarters, so that’s about 0.8% of all disability claims. If we say that half the country has had Covid, then if Covid-related disability claims correspond with Covid-related disability, that means getting Covid raises your chances of claiming disability within a year by 1.6%. If some such cases don’t cite Covid, it could be more, and if some people are using Covid as a false justification (either intentionally or unintentionally), it’s less. I can think of other factors as well but the effect here is so small I’m not going to worry about them.
It’s fair to care a non-zero amount about something that causes a 1.6% rise in chances of disability within the year, but this does not rise to the level of ‘distort my life for months or years to avoid this.’ If Long Covid was causing several percent of people who get Covid to have a long-term inability to work, also known as disability, it would be a lot more than 1% of new disability claims.
Finally, she offers this:
This meta-analysis of 81 studies I mentioned earlier also looked at work: “29.0% and 47.4% of those who were employed premorbidly were not able to return to work”; “5% to 90% were unable to reach their pre-COVID employment level” (p. 128) (As noted earlier, a lot of the studies in the meta-analysis seem to be small n, involving hospitalized people, without controls, and I don’t know what they did about this. Also, it’s possible I’m misunderstanding what group the meta-analysis is about, given how crazy high the numbers are).
Feels kind of grim to call these people ‘employed premorbidly.’ Academic writing is so bizarre, and also those are some of the broadest ranges I’ve ever seen and the control problem seems extreme, so it seems like this is a case of having to read the paper.
The results claimed are certainly large and in charge.
The literature search yielded 10,979 studies, and 81 studies were selected for inclusion. The fatigue meta-analysis comprised 68 studies, the cognitive impairment meta-analysis comprised 43 studies, and 48 studies were included in the narrative synthesis. Meta-analysis revealed that the proportion of individuals experiencing fatigue 12 or more weeks following COVID-19 diagnosis was 0.32 (95% CI, 0.27, 0.37; p < 0.001; n = 25,268; I2 = 99.1%). The proportion of individuals exhibiting cognitive impairment was 0.22 (95% CI, 0.17, 0.28; p < 0.001; n = 13,232; I2 = 98.0). Moreover, narrative synthesis revealed elevations in proinflammatory markers and considerable functional impairment in a subset of individuals.
After three months, they’re claiming one third had fatigue and one in five were cognitively impaired. As I’ve noted in the past when discussing many similar studies (some of which likely got into this analysis) proper controls are key. This includes controlling for perception. That all goes double now given my quick survey found such high rates of impairment in the general population at an arbitrary time.
In the studies I’ve previously examined, there were a few that had very strong controls and found little or no Long Covid effect, and a lot that had little or no controls and found strong Long Covid effects.
Looking at their criteria for inclusion, I see the requirement that Covid diagnosis was confirmed, which is good and was not always present in studies I have seen, but I see zero mention of controls of any kind. The list of studies doesn’t mention their controls, nor do the exclusions. So looks like their control strategy was not to have one?
And, well, yeah.
3.3. Methodological quality and risk of bias
Taken together, the NOS rating of the component studies was moderate, evidenced by mean scores of 6.0 out of 9.0 for prospective/ambidirectional cohort studies, 4.1 out of 6.0 for retrospective cohort studies, and 5.6 out of 9.0 for cross-sectional studies. Common methodological limitations were the failure to include a non-exposed group in cohort studies, failure to ascertain whether outcomes were present prior to COVID-19 infection, and a lack of sample size justification in cross-sectional studies. NOS scores within each category for all component studies organised by design are included (Table S1 in the supplementary material).
Their discussion section gives one way to interpret all this.
Herein we identified that approximately a third of individuals experienced persistent fatigue and over a fifth of individuals exhibited cognitive impairment 12 or more weeks following confirmed COVID-19 diagnosis. Similar incidences of fatigue and cognitive impairment, respectively, were observed amongst hospitalized and non-hospitalized populations. Furthermore, in contradistinction to other persistent symptoms which may be self-limiting (e.g., anosmia) (Hopkins et al., 2020), fatigue and cognitive impairment appear to endure and may potentially worsen over time in susceptible individuals (Jason et al., 2021), as evidenced by similar proportions of affected individuals at <6 and ≥6 months follow-up.
A lower incidence of fatigue and cognitive impairment, respectively, were identified amongst children as compared to adults.
These are two results that don’t smell right to me at all.
No change in symptom rate over time.
No change in symptom rate based on severity or hospitalization.
Those make perfect sense if the symptoms are unrelated to Covid. They don’t make much sense if this is a Covid-related problem, or match the anecdata where people do mostly get better after a while, which I’ve heard from a number of sources anecdotally.
They have a good limitations section where they point most of this out as potential issues, including pointing out that changed world conditions could be causing the increase in symptoms, such as via increased depression. The difference is that they have the attitude that it’s all fine and don’t seem much bothered by not having controls.
Without controls, given all the other data I have, I don’t feel like this tells us much we didn’t already know.
Some harder to interpret data about long covid sufferers in particular (where I’m not sure how many people count as that) still suggests pretty major issues:
Matt bell says that this UK data-set has ~18% of non-hospitalized long covid sufferers with “activities limited a lot.”
The way that data set is presented is infuriating – there are tables that list raw counts without reference to the sample size (maybe it’s an estimated raw number for the whole country, in which case they’re quite small), and tables that are missing the obvious things to be curious about, and so on.
Table 4 estimates that 2.06% of the UK has self-reported Long Covid of any duration on 2 January, and again I presume a majority have had Covid at this point.
Here’s an interesting section, the percent is estimated percent reporting Long Covid.
I presume this is listing their health conditions before Covid since it makes no sense the other way, but am still somewhat confused.
Here’s the start of table 5, including the age distribution since we should put that somewhere.
The dramatic decline for those over 70 is weird, the death rate isn’t that high. What’s even stranger is this is now people who had Covid over 12 weeks ago, instead of the general population, and the estimate has gone down – 2.06% to 1.46%. And then in Table 6 for 12 months the number is down to 0.86%, seeming to contradict the meta-study that said symptoms don’t go away over time, adding to my inclination to dismiss the meta-study as suspected nonsense.
Here is it broken down by symptom, for the general population group with an overall 2.06% estimated base rate of Long Covid.
So there’s a lot of clustering if this adds up to 2%, and also I’d love to see the control group except there doesn’t seem to be one. And always compare to the baseline, for example from Google:
There are approximately 45 million Americans complaining of headaches each year. That works out to about one in every six people or 16.54% of the population. More than eight million Americans visit their doctor for complaints of headache each year.
.,..
The prevalence of fatigue in the general population has been reported to range from 7% to 45% (see 1, 2); a recent study found that 38% of US workers reported being fatigued (2).
An additional 1% isn’t nothing, but correlation of self-reported claims of that magnitude again does not seem like it should panic us.
So in summary: Do we see evidence of the types of sweeping changes we’d expect to see if several percent of people are suddenly unable to work? No, we don’t. We do have newspaper stories about such individuals, but it’s plane crash style coverage rather than auto accident style coverage.
I have long been skeptical that such big statistical effects were happening without being noticed more. I continue to be skeptical.
But Katja’s next section challenges this.
E. Other people’s previous back of the envelope calculations on this are not reassuring.
“If you’re a 35 year old woman, and your risk of ending up with lifelong long COVID from catching COVID is 2.8%, then catching COVID would be the same, statistically speaking, as losing (50 years * 0.18 * 0.028 * 365 days/year) = ~90 days of your life.”
“Your chance of really bad debilitating lifelong Long COVID, conditional on getting COVID, is probably somewhere between a few tenths of a percent, and a few percent.”
Matt Bell was referencing the UK data set above so I have noidea how he can get 2.8%, and in fact my reading of the link says he has it somewhat lower than that but still strangely high.
Scott’s post is Scott’s, so it deserves more careful attention once I’m finished with Katja’s. I agree the conclusions here are not reassuring if we take them at face value, although we’ve already spent several percent of my expected remaining lifespan hiding from this thing, so one could multiply (while remembering that neither is infection fully preventable nor otherwise assured.)
F. Having ‘survived’ covid looks associated with a 60% increased risk of death (after surviving covid) during the following six months
According to a massive controlled study published in Nature (more readable summary here). It also looks like they are saying that this is for non-hospitalized covid patients, though the paper is confusing to me.
Death is different from other things. This is no self-report, also the control in this study is actually trying and the effect size seems large.
The excess death was estimated at 8.39 (7.09–9.58) per 1,000 patients with COVID-19 at 6 months. Individuals with COVID-19 had a higher risk of requiring outpatient care (hazard ratio of 1.20 (1.19–1.21)), at an excess burden of 33.22 (30.89–35.58; all excess burdens are given per 1,000 patients with COVID-19 at 6 months) and at a greater frequency of 0.47 (0.44–0.49) additional encounters every 30 days (Extended Data Table 2b, c).
As Katja notes, the deaths are noteworthy not only because death (0.8% of the time) but also because dying a lot usually indicates something very wrong otherwise.
And then there’s this, which is a question I was going to ask about.
In addition to testing negative-outcome controls (Extended data Table 2a) and to further test the robustness of our approach, we developed and tested a pair of negative-exposure controls. We posited that exposure to influenza vaccination in odd- and even-numbered months between 1 October 2017 and 30 September 2019 should be associated with similar risks of clinical outcomes. We therefore tested associations between exposure to influenza vaccine in even- (n = 762,039) versus odd- (n = 599,981) numbered months and the full complement of 821 high-dimensional clinical outcomes considered in this study (including all diagnoses, medications and laboratory test results). We used the same data sources, cohort-building algorithm, variable definitions, analytical approach (including weighting method) and outcome specification, as well as a similar length of follow-up and interpretation method. Our results showed that none of the associations met the threshold of significance (P < 6.57 × 10−5) considered in this study (Supplementary Fig. 6, Supplementary Tables 22–24).
Incidentally, you have to love when the P value threshold chosen is 0.0000657.
So the same thing didn’t happen with influenza. That rules out or makes more difficult a bunch of potential explanations that revolve around the controls being inadequate.
The patients had a high rate of stroke and other nervous system ailments; mental health problems such as depression; the onset of diabetes; heart disease and other coronary problems; diarrhea and digestive disorders; kidney disease; blood clots; joint pain; hair loss; and general fatigue.
Patients often had clusters of these ailments. And the more severe the case of COVID-19, the higher the chance of long-term health problems, the study said.
So basically everything, including hair loss. One naturally suspects that this has to do with Covid having an easier time infecting those in generally poor health in various ways, or Covid having an easier time being sufficiently symptomatic to get noticed.
Note that severity did matter here. The more severe the case, the more problems (which would also be true if these were underlying problems being selected for). And since this excludes hospitalizations, that implies the missing cases would bring these averages up.
And since we’re talking about so many Covid cases, this would need to very much show up on the excess death tables, within an order of magnitude of the Covid deaths themselves.
The weird thing is that the magnitude of these effects doesn’t seem compatible with the UK estimates or others that say a few percent chance of problems. This is an 0.8% chance of outright death, and a lot of other stuff short of that, and the period after six months presumably adds more than that. So if the majority of the nation has had Covid, that would imply over a million excess deaths on top of recorded Covid deaths, although perhaps moderately less if we factor in severity.
How much excess mortality did we in fact observe?
The USA has about 2600 confirmed deaths per million people, and 2740 excess deaths per million people. That does not leave room for this kind of extra death toll, and is exactly what one would expect if this was a null effect, with a small number of missed Covid deaths filling in the gap. This doesn’t rule out that there’s a large effect here, but those extra deaths would have to be compensated for by reduced deaths from other causes missed by the expected death calculation.
One idea I had was to check the early figures. It would take time for Long Covid to result in deaths. So we should see more unexplained excess mortality later in the pandemic, and unexplained missing mortality early to make the math work. Do we see that?
May 3, 2020: 256 excess deaths per million, 213 Covid deaths per million. The opposite effect, likely due to more unidentified cases very early.
August 2, 2020: 582 excess deaths per million, 466.8 Covid deaths per million. Still the opposite effect.
May 30, 2021: 1903 excess deaths per million, 1783 Covid deaths per million.
So basically early on there were ‘missing’ deaths unaccounted for, then deaths kept pace. The curves look the same with no evidence of lag, or any longer term effects from various earlier waves.
Thus, I defy the data here. There is not a 60% increased risk of death due to Covid in the six months after infection. We would see it in the population data. Somehow, there’s a statistical artifact here, this is correlation rather than causation, and the controls don’t work right to correct for the problem.
G. Overall deaths from everything have been very unusually high at points in 2021, even in 15-64 age group
So first off, if you add the United States the 0-14 graph is mostly below the 0% mark so let me reiterate one more time that kids really, really don’t die of Covid.
What about all that excess mortality we see here? What we see are the waves of Covid infections. What we do not see are delayed effects from those waves, as I noted earlier.
(The Center Square) – The head of Indianapolis-based insurance company OneAmerica said the death rate is up a stunning 40% from pre-pandemic levels among working-age people.
It’s because the scale is the baseline death rate. Covid kills you at a rate approximately proportional to your age-based risk of other death. Early on before vaccines arrived and for that and other reasons death rates fell, a rule of thumb was that it doubled your chance of dying this year. That’s why most of the graphs look the same.
A 40% jump in working-age deaths implies a lot of people were getting Covid, but doesn’t require there to be lots of mysterious deaths. If we checked only working-age people’s excess mortality versus Covid deaths, I bet we don’t see any divergence from the patterns above. Note that the quote doesn’t say how many such folks officially died from Covid, which seems like a weird omission if the quote was supposed to be about Long Covid.
Note especially the final part of the graphs. We do not see excess deaths at all, but a huge portion of people got Covid in December and early January, and many of them never knew it. No visible effect.
This will get much stronger as we get deep into February and then March. If Omicron raises your chances of death afterwards by a lot, we will know it.
There’s nothing to explain here. This is evidence against Long Covid killing people.
H. Sounds like these things involve various damage throughout body, and my guess is that that ends up being regrettable in ways not captured in ‘hours lost to fatigue this year’
See Nature study in F. I also feel like I’ve seen this a lot, but don’t have that many examples immediately on hand. Here’s one other example, not ideal because note that these are hospitalized younger people:
For people younger than 65 who were hospitalized with COVID-19, the risk of death in the 12 months after the infection was 233% higher than it was for people who did not have the disease, results published in the journal Frontiers in Medicine have shown.
Nearly 80% of all deaths of people in the study who had recovered from COVID-19 in the past 12 months were not due to cardiovascular or respiratory causes, suggesting that the impact of the virus is significant and wide-ranging, even after the initial infection has been fought off.
My guess is that all the symptoms are a spectrum, and if the worst looks like an unbelievable amount of cognitive impairment and a pot pourri of organ dysfunctions, or death post-infection, then probably everyone gets a handful of cognitive impairment and organ dysfunction.
There’s a wide variety of symptoms being checked for here, not merely fatigue, in a very grab-bag kind of fashion that should pick up on most things.
We also deal with mortality directly above, and the 233% higher number referenced here seems obviously driven by selection effects. If you’re hospitalized for Covid while non-elderly, that’s a huge sign you were already unhealthy, and the effect size here is also way too big for anything else. To say essentially ‘oh 80% of deaths after Covid were not from anything Covid seems like it causes, in a similar distribution of causes to deaths of other people, and that simply shows how nefarious and mysterious this problem is’ ignores the obvious hypothesis, which is that those 80% of deaths have very little to do with Covid. Seems like a case of trapped priors.
I. It’s easy to just think about these worst case outcomes, but there are a lot of more probable non-worst case outcomes that would still be a non-negligible bummer.
I see people mostly estimating the worst cases, but my guess is that the more probable non-worst case outcomes (e.g. lesser fatigues and brain fogs, kidney damage, arrhythmias etc), are not nothing.
Sure, agreed as far as it goes. Often, as with Covid prevention, the dust specks are more worrisome than the torture. Many people complain very loudly about how bad various dust specks can be, and I agree that the specks of Covid prevention are the dominant form of damage at this point. However for Long Covid in particular the more severe long hauls seem to be relatively common enough they clearly dominate, and the minor stuff is minor. Not everything is counterintuitive.
J. Future unknowns
Across all diseases, how much of their disutility is obvious in the first two years? Saliently right now: we’ve had Epstein-Barr for ages and only now noticed that it apparently has a ~1/300 chance of causing MS, usually showing up between 20 and 40, long after the virus, and wreaking brutal destruction. I’m not sure whether we would realize how bad HIV was if it had appeared two years ago and lots of people had it, but nobody had had it for more than two years yet.
I think mostly this isn’t right, and also we’ve previously dealt with a lot of coronaviruses. Yes, HIV wouldn’t have shown us how bad it is, but a big hint is that you don’t actually get rid of HIV on your own. So it’s an ongoing infection, which raises our prior that there will be a long-term problem. Epstein-Barr seems like a better parallel, and a ~1/300 chance of that kind of thing is not great, but as far as we know this is pretty unique and we need to divide that by the size of the reference class, at which point it doesn’t seem like that big a concern. Also, given Epstein-Barr has been around for ages, we’d have to apply that same logic to every other disease out there.
That doesn’t mean I think saying ‘Precautionary Principle’ is invalid here. When in doubt, ‘don’t catch the new virus that’s going around even if I don’t have a specific reason why not’ seems like a good principle. But it’s infected a lot of people over two years, so I think it applies a lot less now than it did earlier, and despite that I still have this carrying a lot of the remaining weight in favor of prevention (beyond vaccinations) for the young and healthy.
K. Long covid probably isn’t psychosomatic
A French study found that long covid is barely associated with having had covid according to an antibody test, yet associated with believing one has had covid (which itself is unrelated to the antibody test results).
At first I (and I think others) thought that if this wasn’t some error, then long covid was likely psychosomatic and not caused by physically having covid. But on further thought, that’s totally wrong: this pattern could be caused by beliefs causing illness, but it could also be caused by illness causing beliefs, which obviously happens all the time. That is, people’s guesses about whether they had covid are heavily influenced by their symptoms.
That second interpretation was my read on the paper as well, although with a non-zero amount of the first one. If the result is real, my guess is it’s mostly about people assuming that if they feel fatigue they must have had Covid, rather than primarily people who believe they had Covid therefore thinking themselves into being fatigued.
Neither of those is a reason to worry.
It seems to me that we have other data that basically rules out the possibility that long covid is imaginary (e.g. see Nature study above on laboratory abnormalities and raised death rate). Though psychosomatic illness is weird – my understanding is that it could in principle still be psychosomatic, while yielding measurable physical laboratory abnormalities, though intuitively I’d be fairly surprised to learn that the same new psychosomatic syndrome had gripped millions in the wake of a particular belief they had, and raised their risk of death by half. Maybe I’m missing something here.
If Long Covid was psychosomatic, that might be an argument against testing,but the symptoms are still real. It still counts. To me, the French study is very strong evidence that Long Covid isn’t the big deal it looks like elsewhere, and I already had a very different view than Katja of the other studies – I don’t think that risk of death is real, which is both part of why I think Long Covid is rare, and also puts psychosomatic explanations more into play to the extent it matters. But again, I don’t think that’s a major factor here, and also even if it was, I still say it counts.
In the comments to Katja’s post are some objections to the French study, one of which goes so far as to call it debunked (or in this case bunk, which is oddly the same thing as debunked and the opposite of bunked) because seropositivity is also, in this model, bunk:
That French study is bunk.
Seropositivity is NOT AT ALL a good indicator for having had covid: https://wwwnc.cdc.gov/eid/article/27/9/21-1042_article
It is entirely possible that all those patients who believe they had COVID are right.
Some researchers believe absence of antibodies after infection is positively correlated with long covid (I don’t have a source).
This study is bunk and it’s harmful for adequate treatment of seronegative patients. The psychosomatic narrative has been a lazy answer stifling solid scientific research into illnesses that are not well understood yet.
This is not an objection to only the French study, but to the use of seropositivity at all. I don’t know of another lab option post-hoc, so it’s basically saying all we can do is use the PCR test at the time.
So first off, no, it is very much not possible that all those patients are correct, that’s obvious nonsense even before I read the paper. If you ask for self-reports then of course some number of people are going to report incorrect perceptions, regardless of the accuracy of the test.
It’s still important to know if the test is garbage, but before looking at the paper, I’ll note that the test result did correlate in the study with loss of taste and smell, which means it definitely also correlated with Covid. It did not correlate with other symptoms. So in order for this to be true, other long Covid symptoms would need to strongly correlate with the test not working – the test simply not being that accurate is insufficient here even if true.
The study found that only 46 of 72 people (not that many but we use what we’ve got) with positive PCR tests were positive for antibodies three weeks or more afterwards. Being younger or having higher Ct levels made antibodies less likely to be present.
However, seronegative persons were on average 10 (95% CI 3–17) years younger than seropositive persons (Figure 1, panel A) and exhibited RT-PCR Ct values that were 11 (95% CI 8–14) cycles higher (Figure 1, panel B). Moreover, logistic regression showed a precipitous decline in the probability of seroconversion at higher Ct values (Figure 2). For example, a Ct of 35 predicted only a 15% (95% CI 5%–37%) probability of seroconversion, which decreased further with increasing Ct values. Thus, low nasopharyngeal viral loads seem insufficient to elicit a systemic antibody response.
High Ct levels not leading to persistent antibodies makes sense, as this should be a combination of false positives and mild cases, neither of which seem likely to motivate the body to keep antibodies around. The false positives of course are then ‘true negatives’ in the antibody test.
The whole effect here is from mild cases. The correlation is no joke, it’s more like the entire ballgame. Sufficiently mild cases don’t show up, non-mild cases always do:
This FAQ about Ct scores explains that numbers in the 30s can easily not represent a meaningful infection.
7. What can CT values tell us? Samples with CT values <32 generally contain sufficient genetic material for WGS and are more likely to contain replication competent virus. Although there are limitations in the use of CT values, they are one factor to consider when evaluating molecular test results and can be useful in assessing the trend in the viral load. If there is high suspicion of a new infection, laboratories may attempt WGS on samples with CT value <32.
Several studies have correlated Ct values with the presence or absence of infectious virus detectable in culture [3]. One report from Canada’s National Microbiology Laboratory (CNML) observed that PCR positive respiratory specimens with Ct values >24 were viral culture negative [4]. In comparison, the United States Centers for Disease Control and Prevention (CDC) reported that attempts to recover SARS-CoV-2 in culture of upper airway samples was generally unsuccessful when their assay Ct values were >35 (unpublished).
Thus, I find the most logical explanation for this ‘PCR tests that didn’t lead to antibodies were mostly because the person never had Covid and we need to be using a PCR threshold of more like 28-30 and using 40 is just silly.’
Similarly, the French study itself says this about accuracy of the test, with this source that has much bigger samples:
A test was considered positive for SARS-CoV-2 when the results indicated an optical density ratio of 1.1 or greater (sensitivity, 87%; specificity, 97.5%).
We also have this analysis from Bucky, which had a critique I find more interesting.
My favorite part isn’t the critique though, it’s that they gave the serology tests back to the subjects before asking whether they had Covid and everyone basically ignored them and said (best imagined with a heavy French accent) ‘yes, we saw your test and we choose to ignore it.’
Of everyone who had a positive serology results, only 41.5% replied that they thought they’d had COVID. Of everyone who thought they’d had COVID, 50.4% had had a negative serology result.
So we know from the other study’s chart that these are some very stubborn people. If you get a positive serology test in this context, oh yes you had Covid. The people with Ct scores that were very high still didn’t have antibodies (12 of 12 and 17 of 18). The idea that the majority of these people still didn’t think they had Covid is super strong evidence that half the cases were even back then missed entirely, and also that such people simply didn’t care about the serology results. If you’d shown me a positive serology test in January 2021 and asked me if I’d had Covid, I’d have said yes, because you just showed me the test, so I guess I must have.
The French public did not think this way.
I find that to be an interesting study result in its own right. People simply don’t believe such tests, or don’t even care enough to look at them in context.
Check this header out on its own:
So people were 1.8% likely to report having been positive if the test was negative versus 41% if the test was positive. 1.8% is lizardman territory.
But Bucky’s point is that:
Long Covid correlated with reported Covid-19.
If you control for reported Covid-19, the serology result no longer predicts long Covid.
However, if you ignore people’s self-reports and simply look at serology versus symptom reports, we still get increased levels of symptoms.
It doesn’t matter that people have weird ideas about whether they got Covid that are caused by later problems, you can ignore that.
Interesting. So model 1 here looks only at beliefs, model 2 at serology, model 3 at both.
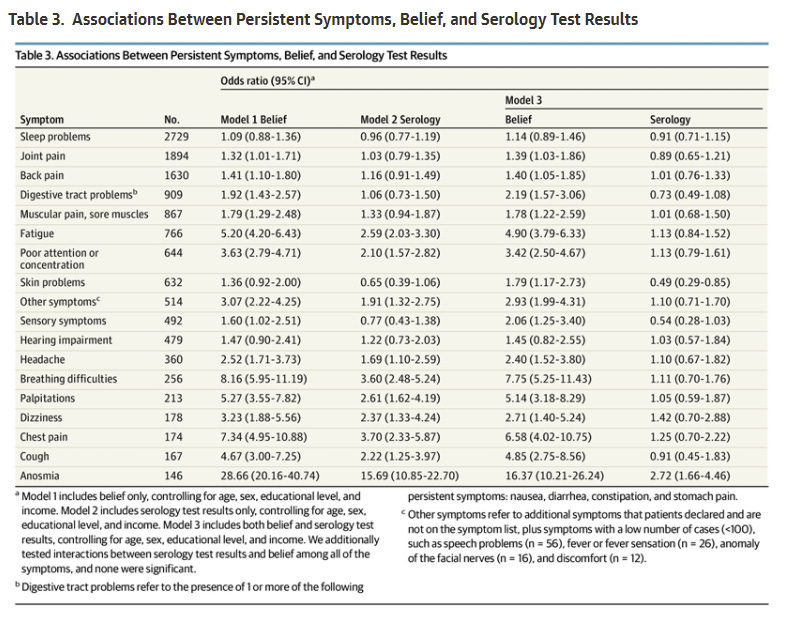
In model 2, which ignores belief entirely, we still do get a bunch of increased risks purely from a positive serology result. In every case, belief is a much better predictor of reported symptoms, again strongly suggesting the model that symptoms cause belief in having had Covid, and perhaps that belief in having had Covid causes symptoms as well. And once we control for belief, serology tells us exactly nothing except for anosmia which is so tightly bound to Covid that the correlation remains even though belief correlates that much better.
Also, there’s Table 2 to look at the raw data.
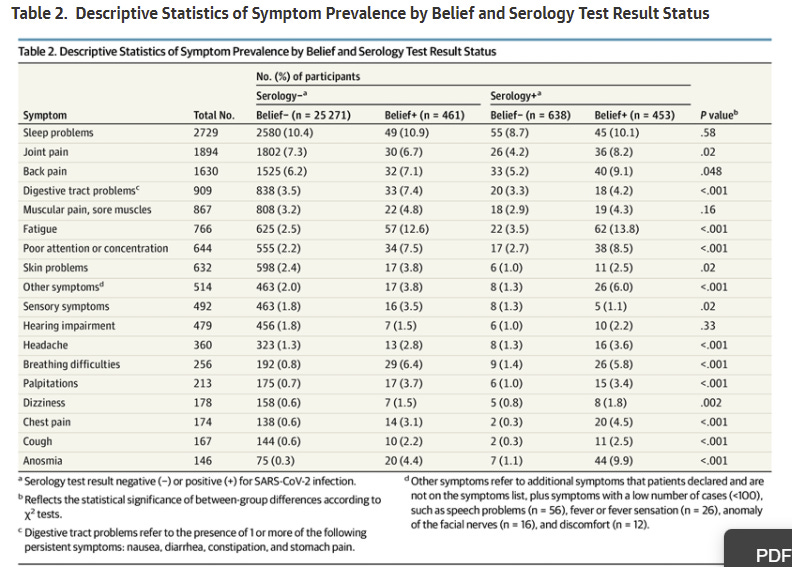
We see some weird stuff here. Conditional on disbelief in having had Covid, positive serology reduces how often people experienced all the common problems except fatigue and poor attention or concentration, with also noticeable increase in breathing difficulties, but that’s it. This makes some sense, in that if you both have the issue and also had Covid, then you’re really likely to notice you had it, whereas if you didn’t actually have it and also have a negative serology test in hand, there are presumably some barriers to fooling yourself.
One thing to note is that there are a number of symptoms where the worst-off group are serology negative but belief positive: Digestive problems, muscular pain, skin problems, sensory symptoms, breathing difficulties. This to me is very strong evidence that the belief-positive group is largely telling a story based on their symptoms.
Model 2 results show that the likelihoods of experiencing the following persistent symptoms are increased by having had COVID (odds ratio / percentage point increase vs serology negative):
Fatigue (2.59 / 5.0%)
Anosmia (15.69 / 4.3%)
Poor attention/concentration (2.10 / 2.8%)
Breathing difficulties (3.60 / 2.3%)
Chest pain (3.70 / 1.4%)
Palpitations (2.61 / 1.2%)
Headache (1.69 / 0.9%)
Dizziness (2.37 / 0.6%)
Cough (2.22 / 0.6%)
Other symptoms (1.91 / 1.3%)
If we add all the percentage point increases (i.e. how many more percentage points serology positive participants experienced persistent symptoms vs serology negative participants – data from table 2) then we get 20.3%. So having COVID on average gives you ~0.2 persistent symptoms vs not having COVID, with presumably some people having more than one symptom.
This is roughly in line with Scott’s conclusions in Long COVID: Much more than you wanted to know. The specific symptoms experienced are also in line with that post, so if that post reflects your current understanding of Long COVID then I wouldn’t update much based on this study except to add some more confidence to a couple of the points Scott makes:
2. The prevalence of Long COVID after a mild non-hospital-level case is probably somewhere around 20%, but some of this is pretty mild.
3. The most common symptoms are breathing problems, issues with taste/smell, and fatigue + other cognitive problems.
So I will notice that these two 20% chances are not the same. Even if the symptoms were uncorrelated entirely you would expect only 16% of people to have at least one symptom in the French study, and I have zero doubt all of this highly correlates.
That’s before you adjust for the percentage of the observed effect that is acting through belief in having had Covid, which I don’t doubt is doing real work here. And of course, this is all early-pandemic stuff, and of course there’s still the thing where people who got Covid during these time frames were substantially different from the people who didn’t.
I do find this all convincing to the extent that it shows the French study isn’t contradicting the other studies. We should assume that a large percentage of long Covid observations are based on people thinking they had Covid because they have health problems, and all the rest, but the whole thing doesn’t simply go away this easily.
L. The general discussion of what is going on with people’s brains sounds terrible
I mean, yes, that is a decent summary of half of LessWrong starting from its founding and also the only reasonable conclusion to draw from Twitter or Facebook.
I think I’m about half kidding, people’s brains do not work the way we’d like them to all that often.
The list of different plausible routes to brain damage occurring [from Covid] according to Nature—some brain cells getting broken, some blood restrictions causing little strokes, some immune system attacking your own brain type issues—is one I want very little to do with.
Famously, the worst thing someone with trouble sleeping due to a medical problem can do is type their symptoms into WebMD. Never do this.
Similarly, if someone starts brainstorming around to list all the ways Covid could damage your brain directly and indirectly, and describing them in detail, you are not going to like it, but this should come as no surprise.
Yes, if these things are real, they are very much not fun. but we knew that already. Things that mess people up mostly sound terrible. If someone described all the things that went wrong with you via aging, it would be so much scarier, so once again fund and otherwise support longevity research and all that.
Also, the descriptions here are in hospitalized patients, which is very much not a representative sample of the young. It’s scaremongering whether or not that was the intention. Comparing snapshot levels of ‘toxic chemicals’ in some Covid patients’ brains to levels under Alzheimer’s is the kind of cherry-picked, emotionally-loaded comparison you can’t let bother you.
M. It sounds like covid maybe persists in your body for ages?
Seems like the virus lives throughout your organs long after recovery, based on autopsies, including of mild/asymptomatic covid sufferers (summary, paper).
Based on autopsies of people who died while still infected, they concluded that it ‘can persist for months’ in various places in the body. How could this possibly inform us on whether the virus persists after recovery, when no one studied recovered from Covid? This is the kind of ‘did you know X can in theory do Y?’ that is primarily useful in ghost stories, and seems misleading slash unjustified enough to be on the borders of what is allowed under Bounded Distrust. But something always can do something, which Katja then reads as ‘maybe persists’ in general.
As far as I can tell, no one thinks Covid can spontaneously reemerge after you recover. If no non-humans had Covid, and we cured every human two weeks ago, that would be the end. Again this is not like HIV, where the virus ‘persists in the body’ in the sense of you never curing the disease.
N. Later rounds of covid are probably bad too
This assumes that later covids are basically free, once you’ve done it once, in a way that isn’t true for e.g. crashing your car. My guess is that later bouts are less bad on average, but far from free.
In my survey, of three people with lasting problems who got covid at least twice, one got the problems with the first, one the second, and one said both contributed (though for the last person, the second was around a month ago). Not a great sample size, but seems like strong evidence that second-round long-covid isn’t unheard of.
The one who said both contributed got their second case a month ago and already had severe issues the first time, so this is pretty much a sample size of one.
In addition to being less likely to happen at all (which definitely helps with Long Covid) later bouts are much less likely to be severe. If we have a model where severity is a major input, they’re a lot less bad, as is Omicron.
This all makes me think of the problem of trapped priors. If you think that long Covid is terrible all the time even in young healthy people who shrugged Covid off, you’re going to think that later bouts must be terrible as well. If you think that people generally have a lot of health problems and blame them on Long Covid when they’re primed to do so, you get the opposite conclusion from the same data.
Someone who is already super worried sees reports of bad problems after reinfections and thinks ‘oh reinfections are bad too’ whereas someone who thinks it’s overblown thinks the opposite, that this is evidence that the associations aren’t causal.
Both have a point. Conditional on it being real it got worse, but the probability of it generally being real should go down.
Katja’s survey link is worth looking at if you want to dive deep and can adjust for the frame. It contains what seems like some good real data, although framed in a very non-neutral way. In particular I like that she asked about how much money people would give up in order to not have problems.
Her full sample size was n=57, these are 9 of the 11 reporting ‘ongoing health problems.’
For people with ongoing health issues, given a choice of A) ‘be rid of ongoing covid related health issues and symptoms forever’ or B) an increase in income this year:
For 10% increase in income:
6 would take health, 3 income, 2 N/A
For 50% increase in income:
3 would still take health, 3 would take income
For 200% increase in income:
1 still prefers health, 2 would take income
I am not going to worry much about six people choosing health over a 10% increase in one year’s income – it’s ‘problem goes away forever’ versus a modest, one-time gain. Even 50% of one year’s income is not that big a downside. In addition, one of the things impacted by health problems is income, including the impact to one’s long-term career, so the health ‘pays for itself’ if it is at all a serious issue. None of this is a strong signal that we should be taking huge prevention costs.
I don’t want to be the one person who would give up double their salary, no matter where the problems came from, especially since their willingness to pay might be much higher than that. I’m not so worried about the other eight.
O. It’s not 100% that you will get it.
I’d guess there’s a decent chance you’ll be able avoid it, via reasonable-to-pay costs. For instance, maybe omicron basically brings herd immunity. Maybe rapid tests get more reliable, easy, and cheap. Maybe long covid becomes a bigger concern, and people worry enough to get R0 generally below 1. Or other technologies improve: Fend really does cut covid exhalations massively and is taken up widely, or something like Novid finds a way to be taken up. (Or your path takes you to being a hermit or living in China, or we spend next year hiding in bunkers from cyborg bees, and you are glad you didn’t pay all that covid risk up front for parties that aren’t happening.)
(If we were doing exactly what we are doing so far, but with air purifiers in most buildings, would R0 would have been ¼ instead of ~1, and would it have died out? Is the problem that we are psychologically incapable of maintaining slightly more caution than needed to keep infections steady?)
Are things so predictable?
So this is where I see this kind of thinking as going ‘off the rails.’ Being a hermit or hiding in bunkers from cyborg bees? Sure, living in China is possible, although I doubt it will help that much as time rolls on, it’s not like they can maintain zero Covid forever and if they do that’s an additional reason not to live there even if you have the option under their policies. But the point here seems to be that you might go completely insane and then save on your permanent prevention costs? I mean, yeah, I guess, but that’s very small comfort and impact on the math, and seems like one hell of a permanent cost.
I do expect things to quiet down a lot, but the idea that we might suppress this entirely is essentially impossible due to animals, and permanent prevention efforts are not worth it even if Long Covid is fully real. This is going endemic, and continuing to be paranoid when that happens is where this stops being remotely reasonable in my eyes.
I still support air filters and vaccinations on cost-benefit grounds, but we do not get to make collective decisions as individuals, and no we are not willing to maintain more caution than necessary when levels are not actually risky because why would we choose to do that.
I do agree you’re not close to 100% to get it even if you do nothing at all, and never were. But that’s one of the key arguments against prevention, that you don’t go from 100% to 0%, with intense prevention retroactive efforts you go from 75% to 25% by the end of the Omicron wave or whatnot (numbers not intended to be very precise), which cuts the benefits in half or more. I still stand by Omicron largely not being worth preventing except during the few weeks when it was peaking.
This is also feeling very ‘throw stuff at the wall.’ There’s worry about second infections and also hope that ‘maybe you could never get a first infection’ and that’s part of an overall pattern that’s looking to be terrified, although one could argue that at some point I started looking for ways to not be terrified and it’s two sides of the same coin, so watch out for that.
P. The likelihood of you getting it probably does depend on how bad it is
This is a strange argument that I think goes the other way. If you’re less likely to get Covid the worse it is, because in the worlds where Covid is more dangerous more people do more to prevent its spread, then that makes your forward-looking risk lower.
It also means that we can use the fact of people not caring much now as strong evidence that Long Covid isn’t that big a deal. And that seems right to me.
Basically, if Long Covid was that bad, we’d all know about it through casual observation, it would be far more talked about and central in our culture, and there would be this huge pushback against people declaring the end of the pandemic. Since we don’t see this almost at all among ‘normal people’ it means Long Covid is rare enough that normal people can mostly plausibly act like it’s all fine. That implies low risk.
Q. Getting covid later is probably better than earlier.
So far this trend seems strong: I would rather get covid now than in March 2020. I expect more of this, from better knowledge, medicine, vaccines, and availability of everything we already have.
If I expect to get covid every year for the next five years, adding one more bout now is adding one more especially bad bout in expectation.
I agree with this as far as it goes, but already we’ve waited two years and already things are vastly improved, and this seems like an argument based on accepting that infection now does prevent a large fraction of an infection later if we hold the amount of prevention fixed. If it’s a ‘every year risk down by half’ thing that’s good news but the math this year is still the math this year.
There is one argument against this. It’s better to get Covid while you’re better protected, so if vaccines and boosters fade with time, delaying your infection (which then gives you even better protection) could backfire, if you don’t intend to get continuous booster shots anyway.
Also, this has another implication that I agree with. We see a lot of the Long Covid cases people talk about coming from March 2020, or otherwise from very early. If Long Covid risk per case is already down quite a lot, we can put a reasonable cap on how bad it was in 2020 by looking at population-level graphs, then divide by a lot already. Yes, it would be better to be able to get Paxlovid than not, but we’ve already eliminated most of whatever risk we started with – at a minimum, >50% for Omicron, >50% for vaccination after that, and extra for better detection and treatment.
R. Huge VOI in following behind the crowd, at a safe distance
This is an argument that you don’t want to get it when everyone else is also getting it and I did agree at the time that this was a thing, but I think its thingness has now ended. And I don’t agree with the logic she lists here – I think it was wise because of hospital overload, rather than the benefit of waiting for a whole bunch of in-coming data from everyone else’s cases. We have plenty of data.
Scott Alexander’s Post
Scott’s post has been mentioned a bit already, but there’s a lot more there. His first section is about physical mechanisms, the second starts to get down to calculations.
2. The prevalence of Long COVID after a mild non-hospital-level case is probably somewhere around 20%, but some of this is pretty mild.
He then describes a bunch of studies: Logue et al find symptoms in 33% of patients vs. 5% of controls.
The British Office of National Statistics looks at people with a confirmed Covid test three months ago, and finds that 14% report having Long Covid symptoms, compared to 2% of a no-Covid control group.
Haverfall et al in Sweden found that 26% of people with previous non-hospital-grade Covid, and 9% of a control group, reported Long Covid-esque symptoms after 2 months. After 8 months, this was down to 15% and 3%.
Sudre et al got data from some kind of UK Covid app with four million users. They chose 4,000 who met various criteria and asked them about long Covid symptoms. 13% reported symptoms after a month, and 2% after three months.
Thompson et al get data from a UK longitudinal study. Their headline finding is that between 7.8% and 17% of patients seem to show at least one Long Covid symptom. But they have no control group, so probably it is lower than this. Also, only 1.2% to 4.8% of people say their Long Covid symptoms “impact normal functioning”, which means a lot of people must have some annoying lingering symptoms that don’t really bother them that much.
Scott’s 20% seems to come from something like ‘take a rough median of the excess reporting here’ and to not worry about precision because there’s so much vagueness built into the definition.
Remember that in my casual survey, about 32% of people reported having one of four symptoms right now, with almost zero correlation to previous Covid status.
When I saw the symptoms only showing up in 5% of controls in the Logue study, I thought if anything that’s the weird one, so I looked and the control group is 21 ‘healthy individuals’. So that explains that.
There’s no similar puzzle in study two because it asks about LongCovid specifically.
Third study only counts ‘moderate to severe’ reports in the above comparison, and it’s a good thing it’s of health care workers then because I have literally never met a civilian who ever reported having ‘moderate to severe’ anything that wasn’t living in a pharmaceutical advertisement. This was their result in more detail.
Of the seropositive participants, 8% reported that their long-term symptoms moderately to markedly disrupted their work life, compared with 4% of the seronegative participants (RR, 1.8 [95% CI, 1.2-2.9]); 15% reported their long-term symptoms moderately to markedly disrupted their social life, compared with 6% of the seronegative participants (RR, 2.5 [95% CI, 1.8-3.6]); and 12% reported that their long-term symptoms moderately to markedly disrupted their home life, compared with 5% of the seronegative participants (RR, 2.3 [95% CI, 1.6-3.4]) (Figure). Furthermore, 11% of the seropositive participants reported moderate to marked disruption in any Sheehan Disability Scale category as well as having at least 1 moderate to severe symptom lasting for at least 8 months, compared with 2% of the seronegative participants (RR, 4.5 [95% CI, 2.7-7.3]).
The differences in the different ratios here are interesting.
I will also repost this, from a comment on a previous weekly post:
Via an excellent comment, we have an important discovery about the Long Covid data.
A major source for the previous pessimistic LC estimates, like Scott Alexanders (the UK’s giant ONS survey) published an update of their previous report which looked at a follow-up over a longer time period. Basically they only counted an end to long Covid if there were two consecutive reports of no symptoms, and lots of their respondents had only one report of no symptoms before the study ended, not two, so got counted as persistent cases.
When they went back and updated their numbers, the overall results were substantially lower. This graphic explains their original mistake: The new headline result is 7.5% of Covid-19 patients had ‘some limitation’ of daily activities after 12 weeks if you ask them if they had long Covid-19. If you go by asking if there were any symptoms from a given list, the rate is lower (like 3%). The full reportis here. What’s notable is that a lot of participants reported LC symptoms with no Covid-19 positive test. They break it down by age and sex in the full report, but you should treat these numbers as numbers for mostly double vaxxed AZ and some mixture of single/double vaxxed Pfizer/Moderna for younger groups, since that’s how it worked in the UK.
This is a pretty dumb error, a very dumb way to get a lot of people very scared and destroy a lot of value. Many thanks to the team for correcting the error, whether or not it was intentional and whether or not they should never have made the mistake. And whether or not the mistake was a reasonable one to be making, which it pretty much wasn’t. Error correction is a big deal.
Basically what they did, as far as I can tell, was this: If you report symptoms, that means for now you have Long Covid. If you report no symptoms twice in a row, congratulations, you don’t have long Covid. If you report no symptoms then symptoms, we still assume the symptoms are due to Covid, and you therefore still have Long Covid. If your last report was no symptoms, you’re still considered to have Long Covid until you report in again with no symptoms. A lot of people didn’t feel the second no-symptom report was a terribly urgent thing to be doing. A lot of people simply hadn’t had the chance to report a second time once their symptoms had cleared up. Yet they still counted the period that included their report of no symptoms, as a length of time that they had Long Covid.
To be blunt, they cheated (intentionally or otherwise), it was a massive effect, and we should have caught it, but to my knowledge none of us did. They have now fessed up. If you ask people to pick from a list of common symptoms, only 3% report that they have one. The larger numbers are mostly or entirely what happens when people are asked if there is anything wrong with them at all, and would they like to blame it on Covid-19. Also the percentages declined a lot over time, so chances are few of the cases would be permanent or semi-permanent. Even if you buy one of the larger numbers, this is a substantial improvement. Given how many people have already had Covid if you go by the antibodies present in various populations or what I would otherwise guess, this seems far more plausible, that Long Covid while real is relatively rare.
This kind of thing is very easy to miss, and I would never have found it without the comment.
3. The most common symptoms are breathing problems, issues with taste/smell, and fatigue + other cognitive problems.
And behold the mother of all COVID symptom persistence studies, Amin-Chowdhury et al:
AC&E act as if this is reassuring – their conclusion starts with “most persistent symptoms reported following mild COVID-19 were equally common in cases and controls” – but it really isn’t. Not only does this 8-month-out sample find high levels of the expected problems (fatigue/smell/taste/breathing), but it finds some unexpected ones too. Cases are likelier than controls to have cognitive problems and weird neurological issues. One flaw in this analysis is that it didn’t ask for premorbid functioning, so you can tell a story where unhealthy people are more likely to get COVID than healthy ones (maybe they’re stuck in crowded care homes? Maybe they put less effort into staying healthy in general?) But I don’t think this story is true – how come obviously plausibly COVID linked things (like smell problems) are significant, and obviously-not-COVID-linked things like diarrhea aren’t?
One thing this study does reassure me about is mental health. A lot of people claim that long COVID involves various mental health sequelae. This study comes out pretty strongly against it. Sure, lots of COVID patients are depressed – but so are equally many controls. The age of COVID is just a depressing time. In fact, it’s kind of weird that you can get this much fatigue, brain fog, etc without an increase in depression diagnoses.
The lack of anything happening in the mental health category jumped out to me as well here. If there’s this many bad symptoms running around and a lot of people have fatigue and brain fog then it’s more than kind of weird not to have depression and loneliness and sadness and frustration follow in their wake. I can tell you right now, if I had severe brain fog, I strongly predict I would be highly frustrated.
4. Sometimes problems go away after a few months, other times they don’t
I mean, yes. Thanks. You can read his descriptions but as far as I can tell this is mostly the throwing up of hands because no one knows. The scary part about chronic fatigue is long-existing chronic fatigue studies in general, not Covid-related.
5. Psychosomatic symptoms probably aren’t the majority of long COVID.
I mean, I’m not seeing too many people claiming that they are. There are a lot more people worried that someone else might be claiming that, than people actually making the claim.
He then reminds us that chronic fatigue syndrome is really bad. I will affirm that I believe chronic fatigue syndrome is really bad, I guess?
The claim I’m making earlier is not that people are ‘making all this up’ or anything, it’s that they are often attributing it to Covid when it’s there for other reasons. That doesn’t make their lives suck less. Nor would it being psychosomatic. Again, still makes life suck. I do think that the French study suggests that something like half and perhaps more of the Long Covid claims are being misattributed.
6. Long COVID is probably rare in children
My overall conclusion here is that long COVID is rarer in children than adults, and may not exist at all. The studies tell us it’s probably somewhere less than 5% of kids, but so far we can’t conclude anything stronger than that.
Note that this is in the model where Scott is defining ‘Long Covid’ so broadly that 20%+ of Covid cases count, so this is a 75%+ reduction. I agree that the evidence here points in the direction of Long Covid being rare in children, and of course that counts as more strong evidence in favor of severity impacting the chances of getting Long Covid, and also some of the details show the dangers of the misattribution problem.
7. Vaccination probably doesn’t change the per-symptomatic-case risk of Long COVID much
He links to this Twitter thread that puts the long Covid rate at 1.04% among breakthrough symptomatic cases, based on self-reports – I worry this link was put in wrong because Scott says it’s complicated but it doesn’t seem like a complicated thread. I’d also note this:
(all this information is from an online poll by a sketchy group of COVID “survivor” activists. But they wrote up their poll in the scientific paper font, as a PDF and everything, so I say we count it anyway)
I can’t tell if he’s joking, not sure if Scott can tell either. I need to use the power of the scientific paper font.
Whereas the next link, this NEJM study, found 19% Long Covid after six weeks by asking about the usual grab bag of symptoms.
Then he says this:
And just before publishing this, someone sent me this study, which very preliminarily finds vaccines might decrease Long COVID risk by a factor of 2. I think a factor of 2-3 is believable; one of 10 or 20, less so.
This seems right to me if we’re talking conditional on symptomatic infection (and bonus points for the title ‘short report on long Covid.’) So I’ll pencil in a factor of two for vaccination conditional on symptomatic infection, in addition to the reduction in risk of such infections in the first place, and in addition to another factor of two (perhaps more) for Omicron.
And finally this:
Weirdly, there are some claims that vaccines can help relieve symptoms of existing long COVID. Sounds kind of like sympathetic magic to me, but the researcher quoted in the linked article said it might “improve symptoms by eliminating any virus or viral remnants left in the body” or by “rebalancing the immune system”. So yeah, sympathetic magic.
I mean worth a shot, I guess?
At one point I linked to this Twitter thread citing 50%-80% reduction in Long Covid symptoms in vaccinated individuals.
8. Your risk of a terrible long COVID outcome conditional on COVID is probably between a few tenths of a percent and a few percent.
This is the big one so I’m going to quote the whole chain of logic.
My original calculation went like this:
About 25% of people who get COVID report long COVID symptoms. About half of those go away after a few months, so 12.5% get persistent symptoms. Suppose that half of those cases (totally made-up number) are very mild and not worth worrying about. Then 6.25% of people who get COVID would have serious long-lasting Long COVID symptoms.
After doing that calculation, I read this essay by Matt Bell, who tries to figure out the same thing. He is much more optimistic. He agrees that about half of long COVID cases go away after a few months, but adds another 50% decrease from “few months” to “lifelong”, kind of on priors, admitting there’s not too much positive evidence for this. Then he adds another factor-of-two decrease from vaccination, based on very preliminary studies from the UK. He estimates that someone with my demographics (vaccinated man in his 30s) has a 2% risk of Long COVID conditional on getting COVID at all. Then he divides by five for the true worst case scenario, based on studies showing that a fifth of people with Long COVID report that it affects their daily activities “a lot”. So by his final number, I have an 0.4% chance of getting really terrible long COVID, conditional on getting COVID at all.
My friend AcesoUnderGlass also did a writeup of this, published after I did my first-draft calculation, which seems to be thinking of this very differently, based entirely on hospitalization rates (which of course are very low in vaccinated people our age). She accordingly concludes that risk is very low. I don’t really understand her reasoning here, but I trust her a lot and am working on trying to converge with her on this.
This sounds a lot like a punt, where the evidence is murky and Scott is simply giving error bounds. Error bounds do seem useful, so let’s see what we can say.
For the (reasonable) upper bound I do think we can start with a 25% chance of ‘any long Covid symptoms at all’ based on symptomatic Covid infection that took place early in the pandemic. This is intentionally a worst-case scenario. Then we can start dividing, and Scott’s logic seems reasonable enough. I can’t imagine less than half of people’s symptoms fading given a reasonable amount of time, and we know that such symptoms only cross this kind of threshold a minority of the time. That would get us to Scott’s 6.25%.
However, that’s symptomatic Covid, and that’s without vaccination or improved treatments, which I think are safely another two divisions by two. And we can add another adjustment for Omicron since almost all forward-looking cases are Omicron, which divides by two again. It’s also without an adjustment for one’s previous health, or a number of other things, but this is an upper bound.
So the pessimistic upper bound would be:
25% base case of anything at all if you’re symptomatic under base conditions
50% reduction from vaccination
50% initial chance of being symptomatic pre-Omicron pre-vaccine
50% reduction from Omicron
50% reduction for chance it doesn’t stick around for long-term
50% reduction for whether ‘it’s as bad as all that.’
Take all of that together and we get a number around 0.8% as a reasonable upper bound.
Another way to get a (reasonable) upper bound is to look at the population-level statistics and ask what we would be noticing on that level, or what matches our observations within our networks, even vaguely, and seems similar.
What should be the (reasonable) lower bound? Very low.
If I wanted to use the above method and keep dividing, I’d adjust the initial 25% to 20% or so, assume that vaccinations cut risk by a factor of 3 rather than 2 especially when we include a booster, assume that two thirds of cases are asymptomatic rather than half even before Omicron, give Omicron credit for a 75% reduction instead of 50% (especially given less reports of loss of taste and smell), and say that half of what we’ve observed is misattribution or needlessly psychosomatic (as in, if you don’t believe in Long Covid it won’t happen in those cases). Then we’d want to adjust for your health, which could easily be another 50%+ reduction for good initial health. And we can cut the ‘it’s as bad as all that’ down from 50% to 20% for the same reason Matt does, and add a 50% reduction for things sticking around forever rather than for the medium-term like Matt does.
So the optimistic-but-not-crazy lower bound would be:
20% base chance of anything at all if you’re symptomatic under base conditions.
66% reduction from vaccination
66% initial chance of being symptomatic pre-Omicron pre-vaccine
75% reduction from Omicron
50% reduction for chance it doesn’t stick around for medium-term
50% reduction for chance it doesn’t stick around for long-term
80% reduction for whether it’s ‘as bad as all that.’
50% reduction for misattribution or unnecessary psychosomatic cases
50% reduction for good initial health and selection impacts
That multiplies to a 0.007% chance, which you’d then have to multiply by the chance you can actually prevent a case moving forward, and which is already well below the ‘ignore this’ threshold. I could find additional excuses to keep going, but the risk of double-counting is a thing and the point has been made.
If I went with conservative numbers as a precautionary principle estimate:
25% chance for literal anything at all, sure, why not.
66% reduction from vaccination plus booster (but requires booster)
50% reduction from being asymptomatic early on and then this went up later, combined with asymptomatic cases not being quite totally safe
50% reduction from Omicron only, on precautionary principle
50% reduction for sticking around
0% reduction from the second sticking around reduction because I’m worried about accidentally double-counting somewhere and want to be safe
60% reduction for ‘as bad as all that’ based among other things on my survey
25% reduction for misattribution to give benefit of the doubt
0% impact of good health
That gets us back to a 0.2% chance of Long Covid conditional on first infection, and less than that less for all future ones combined because of immune strengthening. That’s still the biggest consideration in many cases on whether to care about preventing Covid, but your life is ending one minute at a time.
We can then double back and look at the anecdata and population-level knowledge we have to compare. A 0.2% forward-looking chance for a boosted, essentially healthy person of ‘some serious s***’ seems fully consistent with my observations.
My guess is that the real number is lower, but given uncertainty and precaution I think it’s fair to treat it as about 0.2%.
We then can multiply by the chance of getting Covid in a given year going forward, to see one’s per-year risk. Or we can multiply by the chance of preventing Covid in a given year via ongoing prevention measures you’re considering, and multiply by that to get the benefit of prevention.
Here are Scott’s conclusions:
10. Conclusions
1. Long COVID is many different issues without a common mechanism.
2. Some of these are straightforward and not surprising, eg lung scarring and post-ICU syndrome from severe infection, and would happen in any disease of this severity. Others seem to be more like the poorly-understood postviral syndromes associated with several other diseases. While some symptoms may be psychosomatic, most are probably organic.
3. The three major categories of symptoms are straightforward cardiovascular-pulmonary issues, straightforward smell and taste issues, and more mysterious neurological issues.
Worth noting that Omicron seems to have a lot less issues with loss of taste and smell.
4. Although these get better with time in some people, in a significant number (maybe ~50% of people who had them at six weeks) they persist for as long as anyone has been able to measure them (a few months in the case of COVID, a year or two in the case of comparable syndromes).
5. Post-COVID fatigue is particularly concerning. This would be very bad if we analogized it to CFS/ME, and still pretty bad if we analogized it to other known postviral syndromes. There is no proof that this always gets better over the long term, although no study has looked at them for more than a few years. Facing postviral fatigue on this scale is a new problem.
6. Children probably get Long COVID less than adults, probably at a rate of less than 5% of symptomatic cases. But we don’t know how much less, and we can’t rule out that some children get pretty severe symptoms.
7. Although vaccination decreases the risk of symptomatic COVID, it probably doesn’t decrease the risk of Long COVID per symptomatic COVID case by very much, though it might decrease it by a factor of 2-3.
8. Your chance of really bad debilitating lifelong Long COVID, conditional on getting COVID, is probably somewhere between a few tenths of a percent, and a few percent. Your chance per year of getting it by living a normal lifestyle depends on what you consider a normal lifestyle and on the future course of the pandemic. For me, under reasonable assumptions, it’s probably well below one percent.
EDIT: Here are some other people who tried to do this same analysis. I learned about all of these after I wrote the first draft of this, so you can consider the basic thought process here to be independent of them – but I edited some things to account for what I learned from them before writing the final version.
AcesoUnderGlass: Long COVID Is Not Necessarily Your Biggest Problem
Matt Bell: If You’re Vaccinated, Your Main Risk From The Delta Variant Is Probably Long-Haul COVID
1DaySooner: FAQ: Long-Term Effects of COVID-19
Other Things Of Note
I searched for the term ‘Long Covid’ over all of my weekly posts, to see if I was missing anything important that I’d said previously. Here are the passages that didn’t fit in above but still seem relevant, including to the mindset.
From 9/17/21:
This the latest effort to quantify Long Covid, which I found a link to via LessWrong, with the author thinking of it as similar to chronic fatigue syndrome. There’s enough thoughtful effort here that it needs to be included, but what sticks out at me is the continued reference point shifts in what constitutes Long Covid.
Surveys ask people if they have any symptoms at all, that’s considered Long Covid, then that’s compared to CFS because the most typical symptoms are most typical of CFS. Therefore create association of Long Covid as equivalent to lifelong crippling fatigue. And as usual, I have zero faith in what passes for controls in such measurements. There are then some calculations I’d argue with even given the premise. And if things really were this bad, and a good fraction of a percent of people who got Covid ended up permanently crippled, many of them unable to work normal jobs, I’d point out how many people already did have Covid by this point, it’s at least a large minority of the population. So this seems like the kind of thing that would be impossible to miss on a population level.
On this Washington Post article, 11/18/21:
Then the CDC comes out and says that a full fifty percent of people get Long Covid, with symptoms that persist for at least six months.
If that was actually true, we would know, because a large percentage of the population got Covid-19, so the population statistics would be screaming at us.
There’s this great tidbit: So you’re telling me the percentage is the same at one month as it is at six months, and also two to five months?
This has got to be some sort of fishing expedition for fishing expeditions. My combined update from this week is to move closer to the French study’s position.
The German study, on 12/30/31:
New paper out of Germany. Dashboard link.
I’m surprised that 61.9% of positives had already been caught by PCR. Finally, a control group, and it looks like it controlled for quite a bit. Assuming this is being reported correctly, it’s saying that if you have an unknown infection, you don’t get meaningful Long Covid.
This at least rules out the hypothesis that Long Covid is a threat in asymptomatic cases. If you don’t realize you had Covid, your rate of reporting symptoms doesn’t rise, at least not a substantial amount. We could in theory give the benefit of the doubt that everyone with symptoms got a PCR test, but I’m still awfully suspicious of zero effect, especially when other claims sometimes involved not differentiating much based on severity of the infection.
To the extent that Long Covid is a non-placebo Actual Thing, this seems to strongly suggest that it will indeed scale with the severity of infection, so vaccinations and booster shots will help a lot, and if you’re at low risk for Short Covid (as it were), you’re also therefore not at such high risk for Long Covid either. The idea that children were getting permanently crippled by otherwise harmless infections all over the place doesn’t match this data at all. Long Covid, and the rise in morbidity in the year after Covid infection, are likely the result of Covid infections that get bad and do a bunch of damage.
That also implies that Paxlovid and other early treatments will improve Long Covid outlooks.
There’s a long and good analysis in the Long Covid section of this post from 07/29/21, but it uses a lot of pictures and is long so I’m not copying it over.
The biggest continuing theme is that a lot of times I have had to address scaremongering about Long Covid in children, who are at very little risk.
Conclusion
I did call this The Long Long Covid post for a reason. I put off writing this for too long, but hopefully it will still be of some use. Going forward, I strongly believe that while Long Covid is real and scary and the main thing to worry about in terms of what remains of the pandemic, it is not scary enough that it should cause us to fail to live our lives. The stakes simply aren’t high enough for that, and in particular children are at minimal risk.
I already put my main conclusions up top because of tl;dr, so here I’ll end with an even shorter practical summary.
Children are at minimal risk.
Risk from a given case is proportional to its severity.
One can act as if serious Long Covid will occur in ~0.2% of boosted Covid cases.
That’s not nothing, but it’s not enough that you shouldn’t live your life.
FYI Zvi, insofar as me and my immediate connections are in your network, you may wish to call it three, my mother had it and it took around a year of her life. (She’s mostly on the mend now, which I’m very grateful for.)
My mum got it 29th August 2020. She was nearing 60 at the time.
Thanks for all your effort on this (and the others).
A small point on the following:
That’s one plausible hypothesis, but not what I’d think of as the obvious one: if I’m shown a positive test for X and asked “Do you think you had X?” it’s plausible that I take that to mean “Do you think you had X (for reasons other than the positive test I just showed you)?”. I imagine quite a bit depends on the wording.
It’s quite natural in such situations to assume the questioner is interested in new, non-obvious information. Any inference based on the test result they’ve just shown you doesn’t qualify—unless you assume they’re aiming to test your thinking rather than your health. (of course it’d be handy if we lived in a world where questionnaires contained only precisely worded questions that carefully avoided ambiguity, and respondents interpreted them precisely...)
I’d want to ask the question before and after showing the test result.
I’ve said elsewhere that my hypothesis for this discrepancy is that people think of “had COVID” in terms of a set of experiences, not in terms of viruses/antibodies inside them. If I had a completely asymptomatic COVID infection, did I “have COVID”? I’d probably say yes, but I think it’s very reasonable to say no. The people who had a negative test and said that they did have COVID are slightly more surprising, but perhaps they contracted some other disease and mistakenly attributed all symptoms to COVID.
I agree with the broader point that people give weird answers to survey questions, and seemingly immaterial differences to the survey methodology can yield wildly different answers. I once streamlined a survey by removing 1 click per question and respondents answered 3 times as many questions on average.
If you’re an otherwise healthy young person who has tested positive, what’s the best thing you can do to prevent getting long covid? Seems like there’s research saying that exercising too early can make it worse, but other articles saying good things about exercise, and I’m not sure how to evaluate it.
A rationalist friend of mine told me that the severity of covid increases significantly with the amount of virus particles inhaled. Is this the case? If yes, this might give us reason to use some cheap precautions some more—if not collectively, then on an individual level.
Something I think deserves more attention is the anecdotes suggesting that people infected early on in the pandemic were much more likely to go on to develop long covid than those infected later in the pandemic. I occasionally see this mentioned in the various covid survivor groups on the internet.
To test, I made a poll in the covidlonghaulers subreddit. 55/137=~40% people stated that they were infected in the first wave of infections (before July 2020), even though a look on archive.org suggests that only about 5%* of the subscribers subscribed before this time.
*The earliest they archived a snapshot was actually in August 2020, at which point there had already been quite a few more infections than there were just before July. Some people may have also unsubscribed so I’m not sure what the actual proportion is. I think 5% is a fair-ish estimate since it would also take some time after you get covid and then long covid for you to start looking online for support communities and run into the subreddit. A brief look through the subscriber count over time does suggest that the subreddit has surges of subscribers after surges of infections, so I do think that the temporal link is at least somewhat reliably there and people join the subreddit at a relatively stationary amount of time after getting long covid (i.e. no large surge in popularity of the subreddit unprompted by lack of actual new long covid cases).
I’m glad I found this post, even if late. Thanks for writing this!
There’s a new preprint, pre-vaccine and pre-Omicron, with what seem to be good controls, although based on self-report and the participation rate was low, about 1⁄3, but around that for both cases and controls. This could mean health problems are overreported in both cases and controls or especially cases (if the questionnaire is clearly about COVID), and so possibly overestimate the risk differences. The risk differences between cases and controls for new health problems were pretty big, even larger than Scott’s:
Furthermore:
A risk difference of 2.5%=4%-1.5% for self-reported new medical diagnosis of chronic fatigue syndrome, from figure 2.
A risk difference of 3.2%=9.4%-6.5% for full-time sick leave. (I’m aware 9.4-6.5=2.9, not 3.2. Seems like the authors made a mistake.)
Figure 4 has “Risk differences of symptoms after 6-12 months, comparing SARS-CoV-2 test-positive and test-negative participants, stratified by sex and age group”. I don’t think these are all necessarily new symptoms since catching COVID.
A pessimistic upper bound based on full-time sick leave or CFS could be:
3.2% for full-time sick leave (or CFS).
50% reduction from vaccination
50% initial chance of being symptomatic pre-Omicron pre-vaccine (assuming only symptomatic people get tested)
50% reduction from Omicron
25%? reduction for chance it doesn’t stick around for long-term
I think if you’ve already been diagnosed with CFS, it’s already fairly likely to be long-term.
This gives 0.3%.
If I went with conservative numbers as a precautionary principle estimate:
3.2% for full-time sick leave (or CFS).
66% reduction from vaccination plus booster (but requires booster)
50% reduction from being asymptomatic early on and then this went up later, combined with asymptomatic cases not being quite totally safe
50% reduction from Omicron only, on precautionary principle
33% reduction for sticking around
0% reduction from the second sticking around reduction because I’m worried about accidentally double-counting somewhere and want to be safe
25% reduction for misattribution to give benefit of the doubt
0% impact of good health
This gives 0.134%. Maybe you’d also want to discount more for participation bias, and you could probably make some age and gender adjustments based on Figure 4.
These are both somewhat lower risks than yours, but pretty similar.
Thanks a lot for the post! I’d be curious to hear if people here significantly disagree with your conclusion that “One can act as if serious Long Covid will occur in ~0.2% of boosted Covid cases.”? If so, on what grounds?
This is the UK Office for National Statistics—their usual is to report estimated numbers for the whole country. Easy to miss but it’s in thousands—scroll to the far right of each table with raw numbers and you’ll see that stated near the top. So Table 1 estimates 1,332,000 UK residents with Long COVID, which is in line with the 2% figure stated in Table 4 if we assume that it’s talking about the whole country.
Footnote 7 says “Health/disability status is self-reported by study participants rather than clinically diagnosed. From February 2021 study participants were asked to exclude any symptoms related to COVID-19 when reporting their health/disability status. However, in practice it may be difficult for some participants to separate long COVID symptoms from unrelated exacerbation of pre-existing conditions, so these results should be treated with caution.”
The title of the table can be parsed different ways, but pretty sure that what this table is showing is, “Of people living in private households with self-reported long COVID, what proportion of them say that they first had COVID at least 12 weeks previously” (1.46%). We can see from Footnote 1 that the definition of Long Covid for this study was “Would you describe yourself as having ‘long COVID’, that is, you are still experiencing symptoms more than 4 weeks after you first had COVID-19, that are not explained by something else?” So presumably the remaining 98.54% of people with self-reported long COVID said that they first had COVID at least 4 weeks but less than 12 weeks previously.
The table with the 2.06% is saying, “Of all people in the country, what percentage of them have long COVID of any duration”, i.e., 4 weeks or longer. So I don’t think there’s a contradiction here.
I also tried and failed to figure out how he gets this number.
There is a separate study by the Office for National Statistics with controls (a later one than the one Matt Bell mentions, with different methodology) that I found useful—report is here—though annoyingly it doesn’t break the data down by individual symptoms. Figures 1 and 2 also illustrative with respect to duration of symptoms. The report is pretty comprehensive but the data tables are here, Tables 1-4 show comparisons to controls.
Bottom line is summarized by the points at the top, reproduced below; note that only “Approach 3″ uses self-reported long COVID:
”Approach 1: Prevalence of any symptom at a point in time after infection. Among study participants with COVID-19, 5.0% reported any of 12 common symptoms 12 to 16 weeks after infection; however, prevalence was 3.4% in a control group of participants without a positive test for COVID-19, demonstrating the relative commonness of these symptoms in the population at any given time.
Approach 2: Prevalence of continuous symptoms after infection. Among study participants with COVID-19, 3.0% experienced any of 12 common symptoms for a continuous period of at least 12 weeks from infection, compared with 0.5% in the control group; this estimate of 3.0% is based on a similar approach to the one we published in April 2021 (13.7%), but is substantially lower because of a combination of longer study follow-up time and updated statistical methodology. The corresponding prevalence estimate when considering only participants who were symptomatic at the acute phase of infection was 6.7%.
Approach 3: Prevalence of self-reported long COVID. An estimated 11.7% of study participants with COVID-19 would describe themselves as experiencing long COVID (based on self-classification rather than reporting one of the 12 common symptoms) 12 weeks after infection, and may therefore meet the clinical case definition of post-COVID-19 syndrome, falling to 7.5% when considering long COVID that resulted in limitation to day-to-day activities; these percentages increased to 17.7% and 11.8% respectively when considering only participants who were symptomatic at the acute phase of infection.”
Thank you for this post! One feedback—I found this post much harder to navigate than your other posts (and eventually resorted to summary+bookmark); it is much easier for me to parse/navigate when post sections follow your own line of thinking than when they are structured as replies to sections of other peoples’ posts.
As a very rough estimate, suppose that we value life at $10M and that long covid makes life 10% worse. Then getting long covid is like losing $1M. And in getting covid, there is a 1⁄500 chance of losing that $1M (amongst other things), so an expectation of losing $2k.
So what does this mean for everyday activities like indoor dining? Indoor dining costs something like 5k microcovids, or a 1⁄200 chance of getting covid. Getting covid is bad for reasons other than the possibility of getting long covid, but if we just focus on that long covid component, then it’s a 1⁄200 chance of losing $2k, or an expectation of $10.
On the microCovid math: I noticed right away that number (1/200) didn’t make sense, so I did some quick math. Average American used to eat out 5 times/week, and most people are mostly back to normal. So this would be saying something like 1%-2% of people per week get Covid right now from indoor dining, which doesn’t make any sense, that’s more than double the number of verified cases from all sources. Something screwy there.
Huh, good point. The default assumption for indoor dining on microCOVID is that there are 15 people within 15 feet of you. That seems a little high to me, but going from 15 to 10 only cuts the risk by 50% or so. Not enough to explain it. Even the low end of their confidence interval is around 2k microcovids.
Many americans have (recently) had covid, making them (more or less) immune. That would cut expected microcovids for a random american by some notable factor.
Wait, really? This is a shocking number to me—I assume you got the figure from here or here (I assume both refer to the same study, but neither link to it).
However, this article has data that strongly suggests the real number is much lower (based on this underlying survey).
Core claim:
That is, conditional on being a person who eats out, P(>2-3 times/week) >= 56%. This seems difficult to square with either mean or median person eating out 5 times per week while the 90th percentile is 4-6 times per week.
Yeah I was working super quickly, and Google was being remarkably useless in giving me the actual number of meals so that was the one concrete answer I found. Curious if anyone else has better fu.
I agree 5 sounds like a lot but it’s out of 21 meals so it seems very not-crazy to me. Even if it’s 2, numbers still don’t add up—we don’t see indoor dining restrictions on their own cutting transmission rates by gigantic amounts.
Microcovids start to diverge from actual probabilities earlier than you might think. I’ve commented on their github page
Can you link to your comment?
Long Covid often leads to an inability to do substantial amounts of deep work. Given that a lot of people in this community derive a big part of their self worth from being able to do specific kinds of concentrated work (whether that’s healthy or not) and work sooner counts more than work later,* I think 10% is maybe a bit low. (It depends how quickly you expect Long Covid to improve. If it’s 70% impairment for 2 years, would that translate to “10% of remaining life,” impact-wise?)
*Due to discounting for haste consideration, cognitive decline from eventually getting rigid in one’s thinking, early AI timelines in some people’s cases.
But they don’t look the same, if you include America. (imgur)
Of course, if it’s only about America, it’s probably not about covid. The wave of deaths in the third quarter of 2021 was a lot younger. And they weren’t all registered as covid deaths or pneumonia deaths, as the quote does go on to say. He claims that they are people who had covid months ago, which I’m guessing is an intentional deception. A lot of them are accounted for—as fentanyl deaths.
I think one of the big differences with Matt Bell’s estimate is that the UK study catches asymptomatic cases, so you don’t need to discount for initially asymptomatic vs initially symptomatic cases:
The risk difference for self-reported symptoms 5+ weeks was already ~20% for 25-34 year olds. See this figure, from this page.
This (50% reduction), plus his estimate being for Delta rather than Omicron (50% reduction) could explain most of the differences with your estimates, about 10x lower.
If you use this base figure for your estimates, and don’t adjust for initially asymptomatic vs symptomatic cases, then you’d roughly double your risk estimates.
I appreciate how you balance skepticism with empathy. It took guts. Thank you.
But what about soccer players?
https://stevekirsch.substack.com/p/athlete-collapsesdeaths-following
Isn’t there some evidence?
Just to clarify—given that your first link seems concerned about athlete collapses/deaths following vaccination (supposedly, although the comments there imply insufficient fact-checking), but your second link is about athlete collapses/deaths following COVID-19 infection and your comment is on a post about long COVID, is your concern about heart issues following vaccination or following COVID infection?
If the latter, yes, heart disease and stroke do seem to be more probable following COVID infection according to this recent large study. It should be noted that the control group came from 2017, but the effect sizes they find are so large that it doesn’t seem like differences in average heart disease frequency between 2017 and 2022 in a counterfactual world without COVID are especially relevant.
Thanks for sharing this! It is worrying, but the magnitude does not seem like it would change Zvi’s overall conclusion. Some reasons why:
Not enormous increase in absolute terms. Per the article
Increase in stroke: 0.4% pts
Increase in HF: 1.2% pts
Most participants likely were not vaccinated (looking at the study itself)
162,690 participants who had a positive COVID-19 test between 1 March 2020 and 15 January 2021 were selected into the COVID-19 group
Increase in any cardiovascular outcome for non-hospitalized individuals was 2.85% points (difference of 28.5 cases out of 1000) (Supplementary Table 8 in the study itself)
Stroke is 1.85 / 1000 (0.2% pts), heart failure is 6.05 / 1000 (0.6% pts)
I assume they highlighted stroke and HF because those are particularly severe issues, but eyeballing the table for other scary things (as someone who is not a medical expert): myocardial infarction 0.39, cardiac arrest −0.04, MACE (any major adverse cardiac events) 11.29 (all out of 1000)
Limitation with controls (though I dunno if this is likely to make a significant difference)
Ardehali cautions that the study’s observational nature comes with some limitations. For example, people in the contemporary control group weren’t tested for COVID-19, so it’s possible that some of them actually had mild infections. And because the authors considered only VA patients — a group that’s predominantly white and male — their results might not translate to all populations.
Thanks for digging into this a bit, and I should have linked directly to the paper rather than to an article with the headline “Heart-disease risk soars after COVID” with a focus on relative risks, since as you say the absolute risks are very important for putting things into perspective. For what it’s worth, I agree with Zvi’s final conclusion (“That’s not nothing, but it’s not enough that you shouldn’t live your life”).
That said, an additional 1.2 out of every 100 people experiencing heart failure in the first 12 months after COVID-19 infection, if that holds up in reality, seems like it may have some effects at a population level (suggests that cardiologists will be in more demand, if nothing else). I can imagine that for some people with low risk tolerances, or with high preexisting cardiac risk, it might be a factor in wanting to live one’s life slightly differently than one did prepandemic.
It’d have been nice if they’d included a breakdown of when the vaccinated participants tested positive relative to when they were vaccinated. Supplementary table 21 notes that virtually no one was vaccinated prior to enrollment in the study, but that 62% in the COVID group (56% in the control group) had been vaccinated by the end.
I don’t see a comparison to the base rate (before Covid).
And there are some results
https://www.mdpi.com/1660-4601/18/21/11688/pdf
The trial is under way
https://clinicaltrials.gov/ct2/show/NCT04871867