Note: This post is co-authored with Stacy Li, a PhD student at Berkeley studying aging biology! Highly appreciate all her help in writing, editing, and fact-checking my understanding!
Introduction
The last time I read about aging research deeply was around 2021. The general impression I was getting was that aging research was increasingly more and more funded (good!). Unfortunately, none of the money led to actionable or useful insights (bad).
Over time, you get slightly burnt out by all the negative news.
After getting a job in biotech, I kept a hazy eye on the subject but mostly tuned out of it entirely. But, especially today, I am curious: how has the aging field progressed in the last few years? Since 2021, what has changed?
In this post, I’ll share a list of immediate questions about the state of affairs in aging research, and the answers I’ve found for them. For each question, I’ll offer some basic background knowledge required to understand the question. Feel free to skip that part if you already understand the question!
Did the therapeutic focus on sirtuins amount to much?
Background
Sirtuins are a family of signaling proteins, commonly referred to by their corresponding gene name, SIRT1, SIRT2, all the way up to SIRT7. Their primary role is deacetylation, which is just the removal of a chemical marker (acetyl) on proteins. It was noticed in the 1980s that some sirtuin classes were especially involved in three key activities: modifying histones, which are proteins that tune the accessibility of DNA in the nucleus, transcriptional modification, which determines how DNA is interpreted by the body, and DNA repair, which speaks for itself. And anything involved in modifying and maintaining DNA is something worth paying attention to!
Studies in the 2000s showed that the activity of specific sirtuin classes strongly correlated with age; the young had more sirtuin activity, and the old had less. This seemed to be causative in aging; overexpressing certain sirtuin genes led to lifespan increase and downregulation of them led to lifespan decrease. The results were a bit mixed, and the results were for yeast cells — always a red flag — but there was some promise in viewing sirtuins as an aging target.
It turns out that editing humans to safely overexpress sirtuin genes is somewhat hard to do (as is expressing any gene in humans). But there was an easy way around that: focus on molecules that are required for sirtuin to do its job. A class of therapeutics grew from this: sirtuin-activating compounds.
How do you activate sirtuins?
Well, sirtuins are dependent on NAD+, or nicotinamide adenine dinucleotide, to perform their primary function. Increasing cellular NAD+ levels could also be a way to indirectly push for more sirtuin activity. Practically speaking, NAD+ bioavailability is poor, so supplementation with precursors to NAD+, such as nicotinamide mononucleotide (NMN) and nicotinamide riboside (NR), was instead used. There are plenty of other compounds in this category too: resveratrol, fisetin, and quercetin are all names you may hear mentioned.
How has this fared?
Answer
TLDR: The whole sirtuin theory was losing steam by the time I started reading about it a few years ago. It’s only gotten worse. Nothing particularly useful has come from sirtuin-focused therapies, and likely nothing ever will.
A Cell paper from 2018 found that NAD+ precursor supplementation didn’t improve mice longevity. To be fair, they did show that supplementation improves some aspects of health-span, specifically improved glucose metabolism and reduced oxidative stress to the liver in aged mice, so still potentially useful. But nothing revolutionary. Still, human clinical trials for sirtuin-activating compounds were just beginning around 2021, so there was some nascent hope that something interesting would come from it.
But, as is usually the case, yeast cells aren’t a great model for drugs, and the death of the sirtuin theory has only accelerated upon being exposed to more complex organisms.
A 2023 review of all ongoing NAD+ focused clinical trials found underwhelming results. While it may have promise for diseased populations and helping healthspan (very, very mildly), it doesn’t seem to be the wonder longevity drug that people initially thought it was.
More importantly, per a review paper from 2022, the whole basis of sirtuins as longevity genes is likely fundamentally flawed. This doesn’t mean NAD+ supplementation itself is a bad thing, as it is central to metabolism and has minor benefits, just that the focus on its impact on sirtuins itself have led the field astray. A prescient blog post from 2011 sketches out the bear argument much more deeply.
Have the longevity-focused research institutions/grant programs/startups led to anything significant?
Background
Longevity research was, for a very long time, viewed as near pseudoscience by much of the academic community. It was characterized as having a lack of rigor, being driven by cranks, and generally not being worth most researchers time. Cynthia Kenyon’s pioneering work in the 1990s at UCSF studying the intersection of longevity and caloric restriction changed this. Her work was not only valuable scientifically, but also reputationally amongst academics, elevating longevity research to something more respectable.
But it remained underfunded by federal eyes, partially because aging still wasn’t considered a disease, so NIH grants for it were slim. Researchers focused on aging were forced to apply to tangentially related grants on, for example, Alzheimer’s, and often worried that they’d be rejected due to a lack of background in Alzheimer’s specifically.
As of 2024, that has completely changed. Today, far more NIH grants are dedicated specifically to subfields within aging. While the number of these grants still pales in comparison to diabetes or cancer-related grants, there is far more federal recognition of longevity as a useful scientific topic worthy of study.
There’s also an immense amount of non-federal money flowing in, much of it popping up in the last 3-4 years. Age1 is a VC that focuses purely on longevity startups. Impetus Grants give equity-free money to scientists who are doing longevity projects. Altos Labs, Retro Bio, and NewLimit are all billionaire-backed, for-profit, longevity startups.
Answer
TLDR: No, but it’s a bad question.
After writing the background and pondering on what the answer would be, I’ve realized the question is a bit unfair.
For one, it’s still very early. Good biology research in general can take years, and good aging research can take even longer. Seeing any semblance of an ROI within three years of increased longevity funding is a pipe dream, we should expect it more on the order of ten years.
But, more importantly, it’s hard to tie back funding specific institutions to clinically relevant outcomes, because you never know what the counterfactual would be. Maybe the next big longevity discovery doesn’t come from an aging-focused institution, but rather from a more basic metabolic disorders lab that used a diabetes grant to fund themselves. Does that mean the longevity dollars were wasted? I don’t think so.
Scientific discovery works in strange ways, research from longevity could end up impacting disparate fields from itself, leading to returns in unexpected manners. As long as the research questions being investigated using this influx of money are interesting, I think the money is well spent. And I think those research questions are very interesting.
Unlike the longevity institutions of the past, most of these newer ones have far grander ambitions than interventions like calorie restriction, supplements, and sauna usage. Instead, they focus on areas that, if realized, would yield fundamental step changes in human lifespan. Fields like cryogenics and cellular reprogramming. If there is anybody in the world I’d trust to be given billions of dollars, it’d be smart and ambitious people with that research plan.
Has cellular reprogramming yielded anything useful?
Note: this section genuinely would not be possible if not for Ada Nguyen’s amazing deep-dive on partial cellular reprogramming. Highly recommend reading her article if deeply interested in this topic.
Background
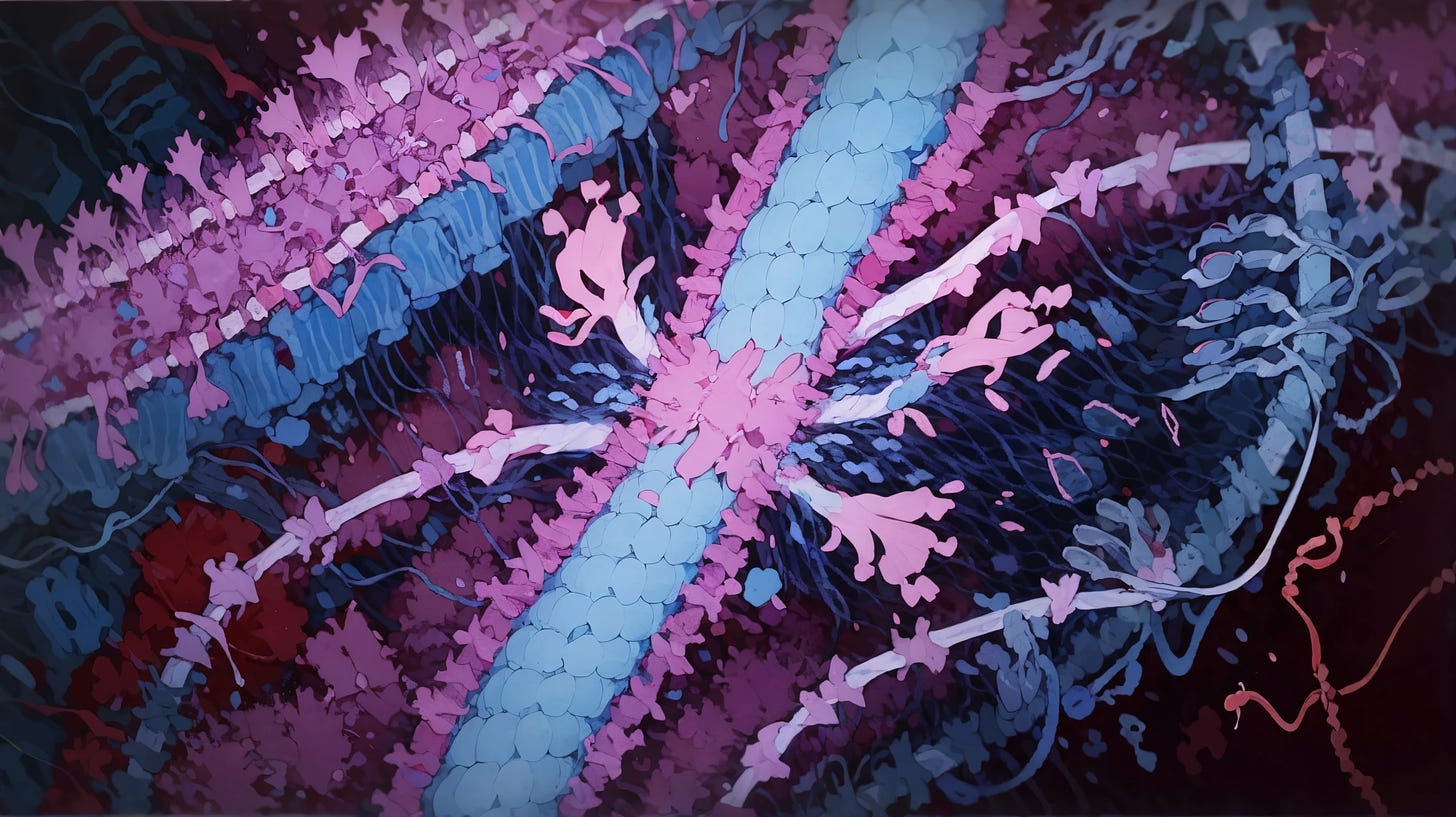
In 2006, Shinya Yamanaka discovered that upon introducing 4 transcription factors (proteins that regulate the DNA→protein process) to skin cells, they would slowly convert themselves to stem cells. These cells were referred to as induced pluripotent stem cells (iPSC’s); induced because it was ‘forced’ to happen by the transcription factors, and pluripotent because they could re-differentiate into any other cell type (heart cell, liver cell, etc). Yamanaka won the 2012 Nobel Prize for this discovery, later deemed ‘cellular reprogramming’.
iPSC’s were somewhat of a revolution in the stem cell field generally because it meant we were able to mass produce stem cells from ordinary cells. While the 4 discovered transcription factors — Oct4, Sox2, Klf4, and c-Myc, also often called OSKM or Yamanaka Factors — weren’t universal across cell types, the concept was. Nearly every cell had a genetic switch for being turned into iPSCs.
But the relevance of iPSC’s to the discussion of longevity has little to do with the ‘stem cell’ part of it. The process by which a differentiated cell turns into a stem cell is gradual, taking weeks. Over this period, as cellular identity is slowly being stripped away, the cell is also rejuvenating on a biochemical level.
Mitochondrial morphology is improved. Epigenetic noise is stripped away. Telomeres are lengthened. And, upon re-differentiation of the iPSC to a cell type, the improvements are retained! One could make an argument that cellular reprogramming leads to age reversal. Is this really age reversal though? Well, we’ll get into that in a second. On the surface though, it does seem like there is something relevant to longevity going on here.
Cellular reprogramming was initially more of a curiosity than something clinically translatable since in-vivo iPSC conversion would be massively disruptive to a complex organism. You could do it ex-vivo; remove cells from a human, allow them to undergo the iPSC conversion + redifferentiation process, and transplant them back in. Unfortunately, that’s infeasible for most tissue types. However the 2016 discovery of partial cellular reprogramming by Ocampo et al. lent fire to the therapeutic potential of this approach.
Typical cellular reprogramming requires cells to be constantly exposed to OSKM over weeks, as the reprogramming process also takes weeks. But if you instead halt exposure to reprogramming factors after just a few days, cells can retain their original identity while still holding onto the rejuvenation benefits. Such a methodology is termed ‘partial cellular reprogramming’. This means that in-vivo cellular reprogramming is a very real possibility and, indeed, has been done.
Quick note: in practice, in-vivo partial cellular reprogramming is done cyclically! The transcription factors are expressed for a few days, turned off (via doxycycline-modifiable promoters) for a few days, and repeated. This allows cells to slowly ‘accrue’ the positive impacts of reprogramming, while also allowing time to recover from the cellular stress of reprogramming, Singular, short doses of transcription factors also have some positive impact, but generally less so than the cyclic approach.
The stage was set for a brand new therapeutic platform based on partial cellular reprogramming and, accordingly, money flowed in. Altos Labs launched in 2022 with $2 billion and backing from Jeff Bezos. Retro Biosciences launched in 2023 with $180 million and backing from Sam Altman. NewLimit launched in 2023 with $40 million and backing from Brian Armstrong. All of them relied on cellular reprogramming being a reliable, robust, and efficacious therapeutic for extending human lifespan.
Of course, as is always the case in biology, there are caveats to the whole approach.
Reprogramming is difficult to do safely. This is related to the delivery problem, but more specific. Even if you can correctly deliver a reprogramming therapy to all the cells in your body, there are tons of medically concerning ‘gotchas!’. As an example, while all cells can be reprogrammed, there are degrees of ‘plasticity’. For example, hepatocytes can be reprogrammed rapidly, while cardiomyocytes take more time. If you go too far with the reprogramming, you get tumors, too little and there’s no benefit. This complicates any attempt to reprogram, as it means each cell type requires a hyper-controlled dosage of reprogramming factors — something that modern medicine isn’t currently capable of. Even localized injection of these transcription factors doesn’t solve this, as most organs and tissues are heterogenous (composed of different cell types).
While in-vivo partial cellular reprogramming improves some known biomarkers of age, they don’t benefit everything. As an example, epigenetic noise is stripped away during reprogramming, but telomere length and DNA mutations stay largely the same. This is especially obvious when you look at the in-vivo results of partial cellular reprogramming. While some papers do report lifespan benefits, it isn’t immortality, more on the order of a 10-20% bump in average lifespan along with a bevy of health-span benefits (increased grip strength, improved body composition, etc). Impressive, but there are facets to aging that are unaffected by cellular reprogramming.
In-vivo delivery of reprogramming therapies is challenging. As with every otherwise promising genetic therapy, getting them to where they need to go is an unsolved problem. Plugging the company I work at, Dyno Therapeutics, as someone trying to solve the issue, but it’s still early days. Nobody yet has a tool that can tack on genetic material into every desired cell in your body, we’re years away from that. The only reliable way to do this in animal models is by editing germ-line cells, but we obviously can’t do that in humans.
Answer
TLDR: Cellular reprogramming has shown promise in animal studies. However no therapies have reached clinical trials yet. One is close though!
There are several promising animal results. One of the strongest results here is an early 2023 study by Macip et al. demonstrating that cyclic expression of transcription factors in wild-type mice could extend their remaining lifespan by 109% when started at a very old age (124 weeks). This translates to 8.86 weeks of life remaining in the control group versus 18.5 weeks for the treatment group. Even more interestingly, they achieved this with AAV-delivered gene therapy! It is as close to ‘how humans would receive the therapy’ as one could get. One of the major caveats about animal studies is that they rarely translate easily to humans, but still! Impressive!
There are a fair number of more concrete concerns with the study, such as the ones detailed here, but the usual concerns with longevity papers aren’t an issue here. The therapy was AAV-delivered, it was done with genetically unmodified animals, and there was a clear + strong signal of lifespan increase instead of a more nebulous ‘biological clock’ decrease. The main issue is just that the sample size wasn’t large enough: only 8 control mice and 12 drugged mice. Overall, it’s an excellent and well-supported result.
Ultimately, for-profit companies are the ones who are going to bring this stuff to the clinic. As of yet, there is nothing within reprogramming that is being actively used in clinical trials. However, one startup is close!
One may expect Rejuvenate Bio, which published the earlier mouse reprogramming paper, to be this one startup. However, judging from news reports, they are focusing more on gene therapy for arrhythmogenic cardiomyopathy, a congenital condition; i.e., not age-related. Longevity still seems to be on their radar, but I’m not seeing much further progress in the whole direction outside of the above paper.
So, if not Rejuvenate Bio, who else?
Turn Biotechnologies. As far as I can tell, they are the only one amongst all reprogramming startups that have something close to the clinic: an injectable drug for dermatology. Interestingly, they also seem to be the only ones with positive results in human cells! It’s entirely ex-vivo, but still, a fair bit closer to translation than anybody else. Even more interestingly, they claim to have solved the delivery problem of transcription factors via ‘nanostructure carriers’. I’m not finding many details on this approach, so we’ll see how well it fares. While results in ex-vivo settings are promising, in-vivo settings are where we’d want a promising drug to have results.
There are other interesting startups in the cellular reprogramming space, but there are relatively few details on their internal progress. There are really only two that have given some very mild insight into what’s internally going on: NewLimit and Altos Labs.
NewLimit gives monthly updates on how their partial cellular reprogramming work is going. They are investing in a high-throughput discovery platform for finding partial reprogramming transcription factors, both from a wet-lab angle and an ML angle. Nothing revolutionary yet, there’s still a lot of set-up work going on internally.
Altos Labs is notoriously private, but I did see a video a bit back about their work on cellular reprogramming. They report a 25% bump in total lifespan alongside some qualitative health-span improvements using a therapeutic based on Yamanaka factors (quoted from the video) across 1000 mice. How impressive is this? It very much depends on their experimental conditions. For example, it depends on what mice they are using. The ‘max lifespan’ statistic can be gamed by using mice with certain genetic disorders, such as Progeria or metabolic conditions, leading to results that don’t necessarily transfer to healthy mice. Looking forward to the full paper on this!
What’s the state of biological clocks?
Background
Biological clocks are a class of methods to utilize biomarker data to predict an individual’s biological age (BA). These models are typically trained on samples with known chronological age (CA): consequently, the difference between an individual’s predicted BA and known CA suggest either acceleration or deceleration of biological aging. In other words, if your biological age is lower than your chronological age, you’re doing great.
Why do we care about biological clocks? For the same reason we care about HbA1c for T2D diabetes patients; we need some sort of clinically relevant and quantitative endpoint if we want to build longevity therapeutics. Why not just use total lifespan? For one, it takes a really long time to assess, but more importantly, it’s a very coarse-grained view of the potential impact of longevity therapeutics. If two drugs both lead to a +5 years in total lifespan, but one operates off preventing tumors and the other operates off of reducing sarcopenia, that’s information you’d like to know! More importantly, that’s information that we need to understand the real underpinnings of biological aging: thus, we have a need for more granular biological clocks.
There are some more easy-to-measure biomarkers on the table; grip strength, graying hair, and wrinkled skin all show strong correlation with age, even within mice and primates! But even this still is coarse, the biological action of a given therapeutic may still be obscured with a phenotype-specific endpoint. Ideally, we’d like something more molecular.
The most commonly discussed biological clocks are epigenetic clocks. The chemical markers that cover your DNA — or epigenetics — affect how it’s converted to RNA, and thus, to proteins. These markers are massively dynamic throughout one’s life, being affected by everything from diet, medications, and even lack of sleep. One of these markers in particular, methyl groups, is highly relevant in estimating biological aging. A 2013 paper by Steve Horvath discovered that methylation sites — often referred to as CpG sites — are connected to age in a relatively simple way. As a creature ages, the ratio of unmethylated CpG to methylated CpG sites goes up, reflecting a general loss of methylation in aging. This is also known as Horvarth’s Clock.
There are several others, but have had a relatively smaller footprint, scientifically speaking. Let’s rattle through them.
Telomere length, the single hallmark of aging that has leaked into popular consciousness, is another way to measure aging. Telomeres are repetitive ‘ends’ on chromosomes, likely meant to serve as a buffer against the inevitably noisy process of cell division. The longer it is, the lower your biological age, or at least that’s what one would hope.
Transcriptomics is another angle. The transcripts, or RNA, in your cells are dynamic to a similar degree as epigenetic markers. Likely even more so! And though it’s not as simple as a ratio of markers to age, like Horvarth’s Clock, or higher-is-better, like telomeres, a mapping from transcripts to biological age may still be possible. And indeed, early results on worms show it is!
Proteomics examines proteins, the end state of transcripts and another potential marker of age. It’s the same story as with transcripts; proteins are important, dynamic, and potentially show a (complex) relationship with age. Again, early results show that they do!
Answer
TLDR: Not great, not terrible. Lots of work left to do. Everyday consumers probably shouldn’t get their biological age tested.
Let’s go through all the methods from above, in the same order.
Epigenetic clocks seem to be useful, but their interpretation is a bit complicated. While we’ve been discussing biological clocks, we’ve unconsciously accepted the axiom that as long as a clock correlates with chronological age, it also correlates with biological age, or, in other words, age-related physiological malfunction. But this isn’t necessarily true! Tree rings correlate with tree age, but don’t seem to match up as closely with the tree actually being worse off. Clocks based on epigenetic ages aren’t dissimilar to this. Clearly, they do correlate with age-related cellular dysfunction. But, depending on how the clock is constructed, they can also be driven by entirely time-based stochastic processes unrelated to cellular dysfunction. Three 2024 papers published in Nature Aging all confirm this; the methylation status of 66 to 75 percent of methylation sites are driven by random processes. More importantly, this trend holds across different independent experiments and explains a large amount of power from pre-existing clocks. To be clear, these methylation changes likely aren’t truly random, but quasi-random: they occur within specific genomic loci and have probable directional changes depending on the system’s initial methylation state. Our current inability to predict or explain these changes makes them appear random, but underlying deterministic mechanisms may exist that we haven’t yet uncovered. Similarly, a 2022 paper confirms that epigenetic age is correlated with some, but not all known cellular hallmarks of aging. All this to say that epigenetics clocks are certainly useful, but their role in giving a clear and simple endpoint for age-reversal therapeutics is fuzzier.
Moving on, telomere length doesn’t actually seem to be predictive of much, so clocks based on it are suspect. A 2022 review reports that the model of telomere shortening as a primary cause of aging has been largely superseded by a model of telomere dysfunction, where telomere damage matters more than length. What is telomere dysfunction, if not shortened lengths? Well, dysfunction is correlated with length, but it has more to do with telomere damage in general, especially chronic damage. This sort of damage, whether that’s due to oxidative stress or something else, can cause persistent inflammation responses. In turn, this leads to aging-esque phenotypes. Notably, this means that even telomeres that are long — relatively-speaking — can still be ‘bad’ telomeres if they had undergone this chronic damage process. All of this implies that relying on telomeres as a biological clock is iffy, since the “history” of a telomere matters and a snapshot won’t tell the full story.
Clocks based on transcripts and proteins have lots of promise and I’m excited to see where they go. There are papers that can draw strong connections between transcripts and protein expression levels to age-related cellular markers of age, organ dysfunction, and mortality risk. There’s a huge amount of papers in this space, with relatively few detractors, so the whole direction does feel quite promising. In a more qualitative sense, there’s also a sense of neatness regarding the mechanism behind why transcript and protein clocks work at all. What is that mechanism? A 2024 review paper covers it in great deal, theorizing that it is the “relative increase of the expression of short genes and a relative decrease of the expression of long genes”. This length-dependence phenomenon repeats across multiple species, is connected to DNA damage — a known marker of age — as longer genes have more DNA available to mutate, and there is some early evidence suggesting a connection to methylation as well. Both the practical and theoretical arguments behind these clocks are strong, but the area is still quite nascent, and future failure modes are always possible. Looking forward to future work!
This is nice! I like seeing all the different subfields of research listed and compared; as a non-medical person I often just hear about one at a time in any given news story, which makes things confusing.
Some other things I hear about in longevity spaces:
- Senescent-cell-based theories and medicines—what’s up with these? This seems like something people were actually trying in humans; any progress, or is this a dud?
- Repurposing essentially random drugs that might have some effect on longevity—most famously the diabetes drug metformin (although people aren’t expecting a very large increase in lifespan from this, rather at best a kind of proof-of-concept), also the immunosuppresant rapamicyn. Anything promising here, or is this all small potatoes compared to more ambitious approaches like cellular reprogramming?
I enjoyed this other LessWrong post trying to investigate root causes of aging, which focuses more on macro-scale problems like atheroschlerosis (although many of these must ultimately driven by some kind of cellular-level problems like proteins getting messed up via oxidization).
Thank you for reading!
Senescent-cell-based therapeutics feels like somewhat of a dead-end...senescence happens for a reason, and clearing out these cells have some second-order downsides. E.g., the inflammation caused by senescence is important for acute injury repair. I am less well-read on this area though!
Metformin and rapamicyn are promising in the same way ozempic is promising; helping curtail metabolic problems helps a LOT of things, but it won’t lead to dramatic changes in lifespan. Definitely in healthspan! But even there, nothing insane.
Imo, partial cellular reprogramming is the only real viable approach we have left, I’m kinda unsure what else the field has to offer if that ends up failing.
But does it work at all?
It seems counterintutive that there would be one single thing called “aging” that would happen everywhere in the body at once; have a single cause or even a small set of causes; be measurable by a single “biological age” number; and be slowed, arrested, or reversed by a single intervention… especially an intervention that didn’t have a million huge side effects. In fact, it seems counterintutive that that would even be approximately true. Biology sucks because everything interacts in ways that aren’t required to have any pattern, and are still inconvenient even when they do have patterns.
How do you even do a meaningful experiment? For example, isn’t NAD+ right smack in the middle of the whole cell energy cycle? So if you do something to NAD+, aren’t you likely to have a huge number of really diverse effects that may or may not be related to aging? If you do that and your endpoint is just life span, how do you tease out useful knowledge? Maybe the sirtuins would have extended life span, but for the unrelated toxic effects of all that NAD+. Or maybe the sirtuins are totally irrelevant to what’s actually going on.
The same sort of thing applies to any wholesale messing with histones and gene expression, via sirtuins or however else. You’re changing everything at once when you do that.
Reprogramming too: you mentioned different kinds of cells responding differently. It seems really un-biological to expect that difference to be limited to how fast the cells “come around”, or the effects to be simply understandable by measuring any manageable number of things or building any manageable mental model.
And there are so many other interactions and complications even outside of the results of experiments. OK, senescent cells and inflammation are needed for wound healing… but I’m pretty sure I don’t heal even as fast at over 60 as I did at say 20, even with lots more senescent cells available and more background inflammation. So something else must be going on.
And then there are the side effects, even if something “works”. For example, isn’t having extra/better telomeres a big convenience if you want to grow up to be a tumor? Especially convenient if you’re part of a human and may have decades to accumulate other tricks, as opposed to part of a mouse and lucky to have a year. How do you measure the total effect of something like that in any way other than full-on long-term observed lifespan and healthspan in actual humans?
And and and...
Still reading and thanks for the write up. Much better than I could do myself and have been thinking it’s time to revisit and see where things stand.
But think this is an obvious type so wanted to mention it for your edit. “In other words, if your biological age is lower than your biological age, you’re doing great.” I assum you mean lower than your chronoloical age there.
So was farther along than I thought. Quick question on the reprogramming aspect. Certainly tissue complexity is a problem when the reaction rates are different and we probably really need to keep something of a balance in general state of cells. Does the interval between cycles of the YF application greatly impact results? You mention a one shot treatment not realy deliering much in the way of benefit so I’m wonder if there an interval period in a cyclic treatement that effectely becomes a bunch of one shot type treatments that are really going no where?
Great catch, dumb mistake on my part, fixed!
As for the latter question, I looked into this, and I think the 2 day ‘on’ of YF expression is literally just the max time it can be expressed without deleterious effects. I think people haven’t investigated the ‘off’ cycle time as much. I suspect people are on the ‘the more reprogramming I can do, the better’ train up until recently, so that level of optimization likely is higher handing fruit.
From here: https://www.nature.com/articles/s41467-024-46020-5
″The currently optimized method of partial reprogramming is the maturation phase partial reprogramming, which necessitates 13 days of continuous expression of Yamanaka factors in vitro...However, this optimized in vitro method may be highly damaging in in vivo models, as a continuous expression of Yamanaka factors for more than 2 days may have lethal effects in mice8,67. In vivo studies now focus on cyclic partial reprogramming....”
The LessWrong Review runs every year to select the posts that have most stood the test of time. This post is not yet eligible for review, but will be at the end of 2025. The top fifty or so posts are featured prominently on the site throughout the year.
Hopefully, the review is better than karma at judging enduring value. If we have accurate prediction markets on the review results, maybe we can have better incentives on LessWrong today. Will this post make the top fifty?